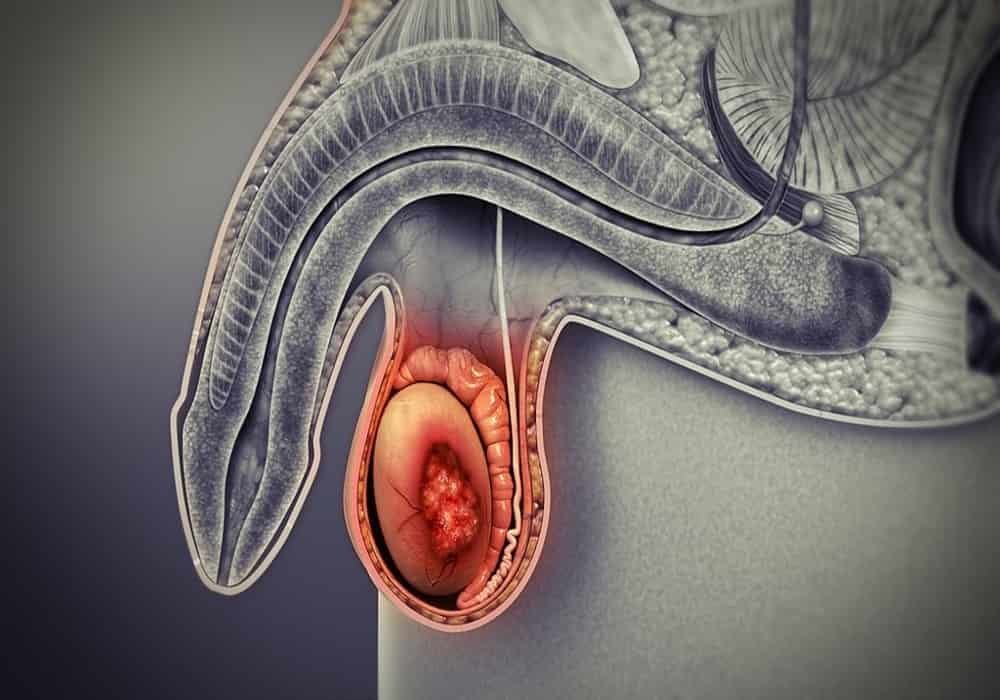
What is testicular cancer?
Testicular cancer starts in the cells of a testicle. Cancerous (malignant) tumor is a group of cancer cells that can invade and destroy nearby tissue. The tumor can also spread (metastasize) to other parts of the body.
The testicles are part of the male reproductive system. These are 2 egg-shaped organs. The testicles are covered with a bag of skin called a scrotum. The scrotum hangs below the penis, between the legs. Each testicle is held in the scrotum by a spermatic cord, a collection of nerves, channels, and blood vessels that enter and exit each testicle. The spermatic cord contains the vas deferens (the channel that circulates semen from the testicle to the urethra), blood vessels, lymphatics, and nerves. The testes make sperm. They also produce a male sex hormone called testosterone.
Risk factors for testicular cancer
A risk factor is something like a behavior, substance or condition that increases the risk of developing cancer. Most cancers are caused by many risk factors. But sometimes testicular cancer appears in men who do not have any of the risk factors described below.
Experts cannot say for sure why the number of new cases of testicular cancer diagnosed each year (incidence) has steadily increased over the past decades. Testicular cancer is the most common cancer in men aged 15 to 29. The number of men diagnosed with testicular cancer is low before puberty, increases significantly after the age of 14, peaks around the age of 30, and decreases until the age of About 60 years old.
Testicular cancer is more common in whites than in men of African or Asian descent. This cancer most often affects men of high socioeconomic status.
The following are risk factors for testicular cancer. Most of the known and possible risk factors cannot be changed. It means you can’t change them. Until we know more about these risk factors, there is no specific way to reduce your risk.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
Finding testicular cancer in its early stages
Finding and treating testicular cancer at an early stage increases the chances of successful treatment. Have a regular check-up and see your doctor if you experience any symptoms or are concerned about your health.
Know your testicles
Every man should be able to recognize the normal appearance of his testicles. Many men discover their testicular cancer on their own by the changes they see in it.
The best time to feel your testicles is right after a hot shower or bath. The heat of the water lowers the testicles and relaxes the scrotum; so it is easier to feel something abnormal when touched.
Carefully palpate each testicle for any changes, such as a lump or tenderness. At the back of each testicle is a tube called the epididymis, which stores and transports sperm. It is normal for this tube to look like a soft string or a small bump to the touch. It is also normal for one testicle to be larger than the other. Comparing the 2 sides may help you spot the differences.
Tell the doctor about any changes as soon as possible. They may then give you tests to identify the cause of the change.
Symptoms of testicular cancer
Testicular cancer may not cause any signs or symptoms in the very early stages of the disease. The signs and symptoms often appear as the tumor grows and causes changes in the body. Other medical conditions can cause the same symptoms as testicular cancer.
See your doctor if you have the following signs or symptoms:
painless lump in the testicle
swelling of a testicle that makes it bigger than usual
pain, which may be dull, in the testicle or scrotum
feeling of heaviness in the scrotum or abdomen
buildup of fluid in the scrotum
back or abdomen pain
tenderness or swelling of the breasts (gynecomastia)
swollen lymph nodes in the neck
difficulty breathing or shortness of breath
cough, sometimes with blood (hemoptysis)
chest pain
difficulty swallowing
swelling in the chest
accumulation of fluid around the lungs (pleural effusion)
weightloss
signs of puberty in boys, such as a deepened voice or hair growth on the face and body, at a younger age than expected
infertility
headache
Diagnosis of testicular cancer
Diagnosis is a process of identifying the cause of a health problem. The diagnostic process for testicular cancer usually begins with a visit to your family doctor. Your doctor will ask you about your symptoms and do a physical exam. Based on this information, your doctor may refer you to a specialist or order tests to check for testicular cancer or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay and normal to worry, but try to remember that other medical conditions can cause testicular cancer-like symptoms. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of testicular cancer.
The following tests are usually used to rule out or diagnose testicular cancer. Many tests that can diagnose cancer are also used to determine the stage, that is, how far the disease has spread. Your doctor may also give you other tests to check your general health and help plan your treatment.
Health history and physical examination
Your health history consists of a checkup of your symptoms, your risks, and any medical events and conditions you may have had in the past. Your doctor will ask you questions about your history:
- symptoms that suggest testicular cancer
- undescended testicle in the scrotum (cryptorchidism)
- testicular cancer
- precancerous condition called germline neoplasia in situ (NGIS)
- Klinefelter syndrome
Your doctor may also ask you questions about your family history:
- testicular cancer
- risk of testicular cancer
- other cancers
The physical exam allows your doctor to look for any signs of testicular cancer. During the physical exam, your doctor may:
- check your testicles for lumps, swelling, hardening or tenderness;
- feel your abdomen, groin and upper chest to see if your lymph nodes are swollen;
- listen to your lungs;
- feel your abdomen to see if any organs are swollen;
- observe your breasts and nipples to see if they are larger and more sensitive.
Ultrasound
In an ultrasound, high-frequency sound waves are used to produce images of parts of the body. The ultrasound is used to confirm the presence of a tumor in the testicle and to check its size and shape, where it is and how strong it is.
The ultrasound can help your doctor differentiate a non-cancerous (benign) tumor from a tumor that is more likely to be cancerous (malignant).
Complete blood count
The complete blood count (CBC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. We do an FSC to assess your general health.
Blood biochemical analyzes
A blood chemistry test measures the level of chemicals in the blood. It makes it possible to evaluate the quality of functioning of certain organs and also to detect anomalies. For testicular cancer, the following blood chemistry tests are done to find out your general health before surgery.
Liver function tests (liver profile) can be used to find the cause of abdominal pain or discomfort. High levels of certain substances in the blood could mean that testicular cancer has spread to the liver.
Kidney function tests are used to check how well the kidneys are doing. They are often done before and after surgery to remove one or both testicles (radical inguinal orchiectomy, or orchiectomy).
Doctors often order blood chemistry tests before treatment for testicular cancer. The rates obtained help establish a base against which to compare future results. This is a benchmark.
Tumor marker tests
A tumor marker is a substance found in the blood, tissue, or fluids taken from the body. If the amount of a certain tumor marker is abnormal, it could mean that a person has testicular cancer.
Tumor marker tests are usually done to see how you react to cancer treatment. They can also be used to diagnose cancer of the testis.
The following tumor markers can be measured for testicular cancer.
Alpha-fetoprotein (AFP) levels are often higher in the presence of a type of testicular cancer called non-seminoma, or non-seminomatous germ cell tumor. AFP levels are never higher in the presence of seminoma, which is another type of testicular cancer.
The level of human chorionic gonadotropin (HCG) may be higher whether you have a seminoma or a non-seminoma. It may also be higher in the presence of liver disease.
Your lactate dehydrogenase (LDH) level may be higher whether you have a seminoma or a non-seminoma. High LDH levels can also mean advanced testicular cancer. Some non-cancerous conditions can also increase LDH levels.
A high level of tumor markers may indicate that the tumor is large, that the cancer is very present in the body, or that it is growing rapidly.
Removal of the testicle
Based on the results of ultrasound and tumor marker tests, the doctor usually knows whether a lump in a testicle is cancerous or not. If the doctor believes the lump is cancer, they will perform an orchiectomy. This surgery removes the entire testicle as well as the spermatic cord. The testicle is removed to make a definitive diagnosis of cancer, and this operation is the first treatment for testicular cancer.
All tissue removed during surgery is sent to the lab. A pathologist will examine it under a microscope to confirm the presence of cancer and to establish what type of cancer it is.
Doctors usually do not use a needle to remove tissue from the testis to find out if a lump is cancerous as this can spread the cancer to the scrotum and lymph nodes in the pelvis.
Removing a testicle sometimes causes fertility problems.
Lymph node dissection
Retroperitoneal lymph node dissection is surgery to remove the lymph nodes located at the back of the abdomen, called the retroperitoneum.
A retroperitoneal lymph node dissection can be done to see if the cancer has spread to these nodes. It is also used to treat certain testicular cancers.
Pulmonary radiography
In an x-ray, low-dose radiation is used to produce images of parts of the body on film. It is used to check for cancer in the lungs and lymph nodes in the chest.
CT scan
A computed tomography (CT) scan uses special x-ray machines to produce 3-dimensional and cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the photos into detailed images.
A CT scan can tell if the cancer has spread to the lymph nodes in the abdomen or chest. It can also tell if testicular cancer has spread to the brain, bones or other organs.
Bone scan
In a bone scan, radioactive materials that attach to the bones (radiopharmaceuticals) and a computer are used to create an image of the bones. It is used to check if the cancer has spread to the bones.
Stages of testicular cancer
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. Information from tests is used to find out how big the tumor is, what parts of the organ have cancer, if the cancer has spread from where it started and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The following staging information applies to germline testicular tumors, which account for over 90% of all testicular cancers. The most frequently used staging system for testicular cancer is the TNM staging system. In the case of testicular cancer, there are 4 stages, ie stage 0 followed by stages 1 to 3. For stages 1 to 3, the Roman numerals I, II and III are often used. But in order to make the text clearer, we will use the Arabic numerals 1, 2 and 3. In general, the higher the stage number, the more cancer has spread. Talk to your doctor if you have questions about staging.
When doctors describe the stage, they can use the words local, regional, or distance. Local means the cancer is only in the testicle and has not spread to other parts of the body. Regional means near or around the testicle. At a distance means in a part of the body farther from the testicle.
To help determine the stage of testicular cancer, doctors also take into consideration the level of certain tumor markers in the blood after surgery to remove the testicle (orchiectomy). If the levels of tumor markers are higher than normal for stage 1 cancer, an S is added at stage which then becomes stage 1S.
Stage 0 (carcinoma in situ)
There is a precancerous condition in the testis called germline neoplasia in situ. It is also called intratubular germline neoplasia.
Stage 1A
The tumor is in the testis and epididymis but may have spread to the inner layer of the membrane around the testis (albuginea). All tumor marker levels are normal.
Stage 1B
The tumor is located in one of the following structures:
it is present in the testis and epididymis and has spread to blood vessels or lymphatics in the testis;
it has invaded the outer layer of the membrane that surrounds the testis (vaginal tunica);
it has invaded the spermatic cord or scrotum and may have spread to blood vessels or lymphatics in the testis.
All tumor marker levels are normal.
Stage 1S
The tumor is found anywhere in the testis, spermatic cord, or scrotum, and 1 or more tumor markers are higher than normal.
Stage 2A
The cancer has spread to 1 or more lymph nodes in the groin, and they are no more than 2 cm in length. The levels of tumor markers may be slightly higher than normal.
Stage 2B
The cancer has spread to 1 or more lymph nodes in the groin, and they are between 2 and 5 cm long. The levels of tumor markers may be slightly higher than normal.
Stage 2C
The cancer has spread to 1 or more lymph nodes in the groin, and they are over 5 cm long. The levels of tumor markers may be slightly higher than normal.
Stage 3A
The cancer has spread to lymph nodes other than in the groin or lungs (distant metastasis). It is also called metastatic testicular cancer. One or more of the tumor marker levels may be slightly higher than normal.
Stage 3B
Cancer has spread to 1 or more lymph nodes in the groin, and 1 or more tumor marker counts are moderately higher than normal.
OR
The cancer has spread to lymph nodes other than the groin or lungs. It is also called metastatic testicular cancer. One or more tumor marker levels are moderately higher than normal.
Stage 3C
Either of the following applies.
The cancer has spread to the lymph nodes in the groin and 1 or more tumor markers are much higher than normal.
The cancer has spread to lymph nodes other than the groin or lungs. It is also called metastatic testicular cancer. One or more levels of tumor markers are much higher than normal.
The cancer has spread to a part of the body far from the tumor other than thelymph nodes or lungs. One or more of the tumor marker levels may be much higher than normal.
Recurrent testicular cancer
Recurrence of testicular cancer means that the cancer comes back after treatment. If it reappears where it first started, it is called a local recurrence. If it reappears in tissues or lymph nodes near where it first started, it is called a regional recurrence. It can also reappear in another part of the body: this is called a recurrence or distant metastasis.
If testicular cancer spreads
Cancer cells can spread from the testis to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer usually grows and spreads helps your healthcare team plan your treatment and future care. If testicular cancer spreads, it can spread to the following parts of the body:
- lymph nodes at the back of the abdomen (retroperitoneal nodes)
- lymph nodes surrounding the main blood vessel of the body (para-aortic nodes)
- lymph nodes distant from the tumor that are located in the pelvis, mediastinum, or base of the neck
- lungs
- liver
- bone
- brain
Prognosis and survival for testicular cancer
If you have testicular cancer, you may be wondering about your prognosis. A prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type of cancer you have, the stage and other characteristics of the disease, the treatments chosen and the response to treatment can review all of this data together with survival statistics. to arrive at a prognosis.
A prognostic factor is an aspect of cancer that a doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. We often discuss prognostic and predictive factors together. They both play a role in choosing the treatment plan and establishing the prognosis.
The following are the prognostic factors for testicular cancer.
Where the cancer started
Non-seminoma that starts in a testis or behind the abdomen, either in the retroperitoneum, has a better prognosis than an extragonadal germ cell tumor that starts in the center of the thorax, between the lungs, or in the mediastinum.
Type of germ cell tumor
Seminomas often respond better to treatment than non-seminomas. Seminomas therefore usually have a better prognosis.
Where the cancer has spread
Testicular cancer that has spread, or metastasized, to organs other than the lungs usually has a poor prognosis. The location of the metastases is the main prognostic factor for seminoma. Doctors also take into consideration the location of the non-seminoma metastasis, but other prognostic factors (such as where it originated and the dosage of tumor markers) are also important for this tumor.
Spread to retroperitoneal lymph nodes
When doctors assess the prognosis, they take into account the number of retroperitoneal lymph nodes affected by cancer and their size.
You are less likely to have testicular cancer coming back (recurring) if:
- less than 6 retroperitoneal lymph nodes are affected by cancer;
- none of the retroperitoneal nodes measure more than 2 cm in diameter;
- the cancer did not penetrate the capsule of the retroperitoneal nodes, so it is not outside the nodes, which is called extranodal extension.
Determination of tumor markers
Doctors consider testing for certain tumor markers in the blood when assessing the prognosis for non-seminoma. A high dosage is linked to a poor prognosis for non-seminoma. The dosage of tumor markers for the seminoma is not taken into account.
International Germ Cell Cancer Consensus Group (IGCCCG) classification system
The International Germ Cell Cancer Consensus Group (IGCCCG) developed a classification system based on prognostic factors. It describes how well the cancer is expected to respond to treatment. This system helps doctors make decisions about treatment for advanced germ cell tumours. It also helps researchers design clinical trials.
IGCCCG divides testicular germ cell tumours into 3 prognosis groups:
| Prognosis group | Seminoma | Non-seminoma |
|---|---|---|
| good | The tumour has only spread to the abdominal lymph nodes or the lungs or both. The alpha-fetoprotein (AFP) level is normal and other tumour markers can be any level. | The primary tumour is only in the testicle or in the back of the abdomen. The tumour has only spread to the abdominal lymph nodes or the lungs or both. All tumour markers are normal or mildly elevated. |
| intermediate | The tumour has spread to organs other than the lungs. The AFP level is normal and other tumour markers can be any level. | The primary tumour is only in the testicle or in the back of the abdomen. The tumour has only spread to the abdominal lymph nodes or the lungs or both. At least one tumour marker level is moderately high. |
| poor | There is no poor prognosis grouping for seminoma testicular cancer. | At least one of the following must be true:
|
Treatments for testicular cancer
If you have testicular cancer, your healthcare team will make a treatment plan just for you. It will be based on your health and specific cancer information. When your healthcare team decides which treatments to offer you, they take the following into consideration:
- the type of germ cell tumor (seminoma or non-seminoma)
- the stage of cancer
- the risk of the cancer coming back (recurrence)
- if you want to get a pregnant woman (fertility)
- what you prefer or want
You may be offered one or more of the following treatments for testicular cancer.
Surgery
The following types of surgeries may be used to treat testicular cancer.
A radical inguinal orchiectomy, or orchiectomy, involves the removal of the testis and the spermatic cord. This is usually the first treatment for testicular cancer, and it removes the cancerous testicle and confirms the diagnosis.
Orchiectomy is the surgical removal of a testicle. It is both diagnostic and therapeutic: orchidectomy confirms the diagnosis of testicular cancer but it is also the first step in the treatment of this tumour. The surgeon makes an incision of a few centimeters in the groin (inguinal incision). He extracts the testicle and sends it to the specialized laboratory which performs an anatomopathological examination. The latter makes it possible to specify the nature of the tumor and directs the doctors towards complementary treatments such as chemotherapy and radiotherapy. The operation lasts from half an hour to an hour and a half; it takes place under general anesthesia or spinal anesthesia (locoregional anesthesia). If the patient wishes, the surgeon replaces the missing testicle during the same operation with a silicone prosthesis. This can also be implemented later.
Retroperitoneal lymph node dissection is surgery to remove the lymph nodes located at the back of the abdomen (retroperitoneum). If we remove the lymph nodes that are on the same side of the body as the tumor, the dissection is ipsilateral. If the lymph nodes are removed on both sides of the retroperitoneum, it is a bilateral dissection. It is possible to perform this surgery at the same time as the orchiectomy or to do it at a different time. Retroperitoneal lymph node dissection may be part of the treatment for early testicular cancer. It can also be used after chemotherapy to treat advanced testicular cancer.
Post-chemotherapy surgery removes the cancer that remains after orchiectomy and chemotherapy. This can be done when the testicular cancer does not respond fully to the chemotherapy given after the orchiectomy. Post-chemotherapy surgery may include bilateral retroperitoneal lymph node dissection.
Metastasis surgery can be done to remove testicular cancer that has spread (metastasized) to the lungs, mediastinum, liver, brain, or neck.
Lymph node dissection
Lumbo-aortic lymph node dissection is a surgical procedure performed by an experienced team which is mainly intended for patients with a non-seminomatous germ cell tumour. It consists in removing, from a midline incision in the abdomen, the lymph nodes located in the abdomen or the thorax which could still be carriers of cancerous cells at the end of the chemotherapy. These are referred to as masses or residual lesions. In fact, these nodes receive lymph from the testicles. They are therefore the first to be affected when the cancer spreads. In the case of cancer of the right testicle, the lymph nodes located to the right of the aorta are removed. In the case of left testicular cancer, the lymph nodes to the left of the aorta are surgically removed. Performed under general anesthesia, the operation is long, it lasts from 2 to 5 hours, and complex.
Chemotherapy
Chemotherapy is commonly used to treat all stages of testicular cancer. It is usually given after an orchiectomy. In general, chemotherapeutic agents are combined.
BEP is the main combination chemotherapy drug used to treat testicular cancer. It includes bleomycin (Blenoxane), etoposide (Vepesid, VP-16) and cisplatin. Doctors may only give etoposide and cisplatin (combined with EP). PE is used when bleomycin affects the lungs (pulmonary toxicity) or if it is highly likely to cause lung damage.
High-dose chemotherapy and a stem cell transplant may be used to treat recurrence of testicular cancer if standard-dose chemotherapy does not work and the cancer comes back (comes back). High doses of carboplatin (Paraplatin, Paraplatin AQ) and etoposide are given. After high-dose chemotherapy, a stem cell transplant is done to replace those that have been damaged or destroyed by high-dose chemotherapy. The stem cells used in the transplant are taken from your blood, called an autologous peripheral blood stem cell transplant.
Radiotherapy
Radiation therapy may be used to treat stage 1 or 2 seminoma after orchiectomy. We opt for external radiotherapy. Radiation is directed to the lymph nodes in the abdomen and pelvis.
As with chemotherapy, we speak of adjuvant radiotherapy because it is carried out after the surgical removal of the testicle(s) in order to limit the risk of recurrence. Radiation therapy involves delivering high-energy rays to the site of the tumor to kill cancer cells. It is used more particularly in men suffering from seminomatous tumours, because the cells of these tumors are particularly sensitive to the action of the rays. This treatment can also be applied to areas of lymph nodes or tumor metastases, five days a week for two to three weeks. The dose delivered depends on the stage of the tumour.
Active surveillance
Active surveillance is the preferred treatment for stage 1 testicular cancer after orchiectomy. The healthcare team is watching for any signs and symptoms that indicate the cancer has come back. Treatment is only given if testicular cancer has come back.
Active Cancer Surveillance and Visits | Monitoring and Follow-up for Cancer Survivors
Fertility disorders
Some treatments for testicular cancer can cause fertility problems, which may affect a man’s ability to father children (make a woman pregnant). Tell your doctor if you want to have children someday. Your doctor may suggest that you store your semen (sperm bank) before you start cancer treatment.
If you cannot or do not want to be treated for cancer
You may want to consider care that aims to make you feel better without treating the cancer itself, perhaps because cancer treatments no longer work, or they are no longer likely to improve your condition, or cause them to work. secondary are difficult to tolerate. Other reasons may explain why you cannot or do not want to receive cancer treatment.
Talk to members of your healthcare team. They can help you choose the care and treatment for advanced cancer.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits, especially during the first 10 years after treatment. These visits allow the healthcare team to monitor your progress and to know how you are recovering from treatment.
Clinical tests
Talk to your doctor about clinical trials for testicular cancer that are underway in your country and are accepting participants. Clinical trials aim to find new methods of preventing, detecting and treating cancer.
Supportive care for testicular cancer
Supportive care empowers people to overcome the physical, practical, emotional and spiritual barriers of testicular cancer. It is an important component of the care of men with this disease. There are many programs and services that help meet the needs and improve the quality of life for these men and their loved ones, especially after treatment is over.
Recovering from testicular cancer and adjusting to life after treatment is different for every man depending on the stage of the cancer, the type of treatment given and many other factors. The end of cancer treatment can lead to mixed emotions. Even if the treatment is finished, there may be other issues that need to be addressed, such as coping with long-term side effects. A man who has been treated for testicular cancer may be concerned about the following.
Self-esteem and body image
Self-esteem is how we feel about ourselves. Body image is how we perceive our own body. Testicular cancer and its treatments can affect a man’s self-esteem and body image.
After surgery in which one or both testicles have been removed, the scrotum appears empty to the eye and to the touch. A man can therefore be preoccupied, anxious and embarrassed. He may also feel less masculine and less attractive. He may also feel uncomfortable around others because of the changes in his body.
Talking about their emotions can help some men adjust to their different body images. Getting the support of other testicular cancer survivors and a professional counselor can be helpful. Reconstruction with a prosthetic testis (artificial testicle) can also help cope with changes in body image and self-esteem.
For many people, body image and how other people look is closely related to self-esteem and can be a source of real concern and significant distress. They may be angry or upset, afraid to go out, or fear being rejected by others, even though the effects of treatment may not be visible.
Sexuality
Many men continue to enjoy strong, supportive relationships and satisfying sex lives after testicular cancer. Cancer cannot be spread through sexual contact between partners.
Removing a testicle by surgery (radical inguinal orchiectomy, or orchiectomy) should not affect a man’s ability to have an erection and ejaculate since the remaining testicle can produce enough testosterone and sperm. Men who have had both testicles removed or have lower than normal testosterone levels after having one testicle removed usually have testosterone replacement therapy given by injection or skin patch.
Some treatments for testicular cancer can cause sexual problems. Retrograde ejaculation and dry orgasm can be caused by retroperitoneal lymph node dissection. Erectile dysfunction can occur during chemotherapy since drugs can lower testosterone levels. It can also be caused by retroperitoneal lymph node dissection and radiation therapy if nerves and blood vessels have been damaged, which affects a man’s ability to have an erection.
Talk to your doctor about sexual problems that come with treatment for testicular cancer and how to manage them. Some men and their partners may need counseling to help them cope with the effects of testicular cancer and its treatment on their sexual relationship.
Fertility
Some treatments for testicular cancer can cause fertility problems, which may affect a man’s ability to have children (make a woman pregnant). Infertility occurs when the testes do not make enough sperm or when the sperm are damaged. Depending on the treatments given, the man’s age and other factors, infertility is temporary or permanent.
Some testicular cancer surgeries can cause permanent infertility. If both testicles are removed (bilateral orchiectomy), the man no longer makes sperm, so he can no longer have children. Retroperitoneal lymph node dissection can also damage nerves, which can make ejaculations retrogrades, therefore the infertile man.
Chemotherapy and radiation therapy can reduce the number of healthy sperm made by the testes. It is usually temporary. Sperm production returns to normal after treatment. It may take up to 2 years after treatment for sperm to return to normal and normal quantity.
If a man ever wants to have children, he may be offered the option of storing his sperm or banking it before treatments such as retroperitoneal lymph node dissection, chemotherapy and radiation therapy. This is because it is difficult to know how these treatments will affect fertility. Semen is collected before treatment in case the sperm count does not return to normal afterwards. It is frozen and stored for future use in a fertilization procedure called artificial insemination.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, American Cancer Society, Web MD, National Health Service (UK), HealthLine, MedlinePlus is a service of the National Library of Medicine (NLM) – part of the National Institutes of Health (NIH), National Center for Biotechnology Information, U.S. National Library of Medicine (NCBI), Gustave Roussy (France), Moffitt Cancer Center
Photo credit: Wikimedia Commons