Multiple Sclerosis (MS)
Multiple sclerosis is an autoimmune disease that attacks the central nervous system. A dysfunction of the immune system leads to lesions that cause motor, sensory, cognitive, visual or even sphincter disturbances (most often urinary and intestinal) until paralysis. It is in this sense, this is potentially disabling disease of the brain and spinal cord (central nervous system).
WHAT IS THE CENTRAL NERVOUS SYSTEM?
The central nervous system is made up of the brain and the spinal cord. It provides intellectual and sensory functions (vision, hearing, taste, etc.), controls and regulates movements and balance, and controls the functioning of muscles. Damage to the central nervous system can therefore result in an anomaly in each of these major functions.
The cells of the central nervous system can be divided into two main families: neurons, which transmit information, and glial cells, whose role is to nourish and maintain neurons. Among the latter, there are cells called oligodendrocytes, which are responsible for the formation of myelin in the central nervous system.
Myelin forms a segmented sheath along axons, extensions of neurons, and acts as an insulator that prevents “short circuits”. The spread of nerve impulses is discontinuous, skipping the myelinated segments, which speeds up transmission. When there is no or no more myelin, as in multiple sclerosis, the spread of nerve impulses is less well. New, thinner myelin sheaths may be reconstituted in some cases.
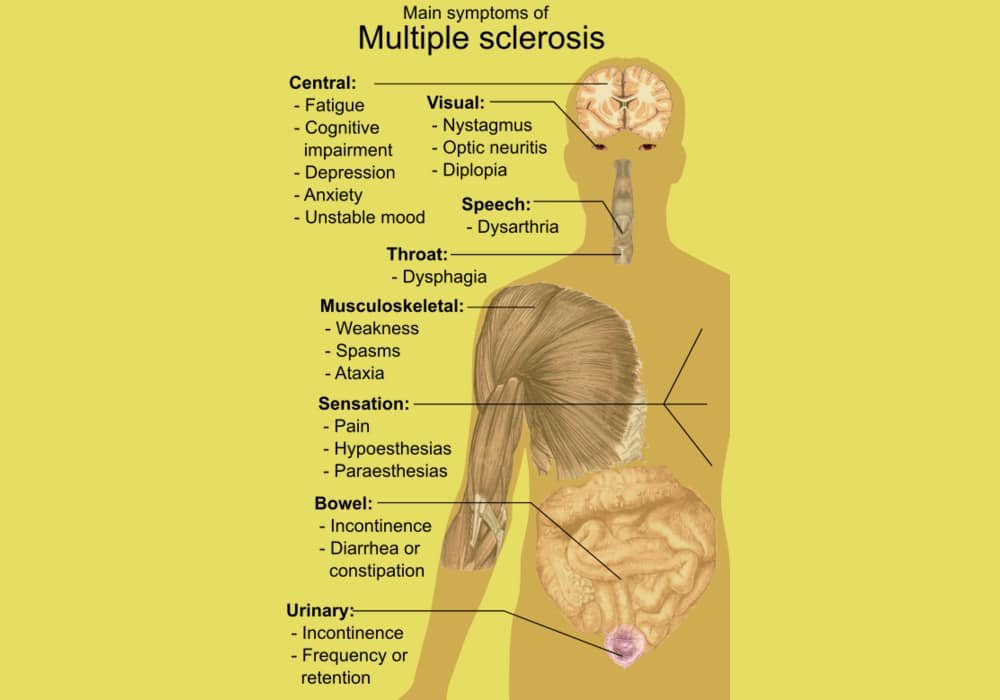
Symptoms of multiple sclerosis
Symptoms depend on the location of the plaques. They vary greatly from person to person, as well as from outbreak to outbreak. Here are the main symptoms that can appear within hours or days:
- Vision problems (double vision, loss of vision usually in one eye at a time). These disorders are caused by optic neuritis (damage to the optic nerve). They are the first symptom in about 25% of cases.
- Abnormal sensations (sensory disturbances): brief pain, tingling or the feeling of electric shocks.
- Numbness or weakness in one or more limbs which may interfere with walking.
- An abnormal fatigue in its intensity.
- Shaking and difficulty controlling movements.
- Loss of balance.
- Muscle spasms or contractures (spasticity), sometimes painful.
The following symptoms, which are less often spoken of, may also occur (especially when the disease progresses).
- Difficulty speaking.
- Urinary incontinence or urinary disorders (urgent urges, difficulty emptying your bladder, urinary tract infections, etc.).
- Constipation.
- Sexual disturbances.
- Partial or total paralysis (of any part of the body).
- Problems with memory, mood (depressive phase) or concentration.
- Having one or more of these symptoms is not sufficient to diagnose multiple sclerosis as they are common with other neurological and other diseases. This is why you should always consult your doctor…
- In some cases, an increase in body temperature (fever, hot bath, physical exertion) can lead to a reactivation of old neurological symptoms, most often vision disturbances, but not only. This transient phenomenon is known as the “Uhthoff phenomenon”. This is not a real flare-up since the symptoms go away when the body temperature drops. Rather, it is a transient blockage of nerve impulses due to heat. Not everyone who has multiple sclerosis is prone to this phenomenon.
People at risk for multiple sclerosis
People with a close relative who have multiple sclerosis have an increased risk of having multiple sclerosis too: the risk goes from 0.1% (in the general population) to 1% to 3% 37. However, multiple sclerosis is not an inherited disease. Several genes could lead to a susceptibility to the disease, that is, an increased risk of developing it. Scientists are also exploring the link between genes and when or how severe the disease is.
Women are three times more often affected than men.
The descendants of North Europeans have a predisposition to multiple sclerosis. The people of Asia, Africa and the indigenous peoples of America are the least affected by the disease.
People who live in a high latitude of the northern hemisphere or the southern hemisphere or who have lived there for the first 15 years of their life. The disease is 5 times more common in northern or temperate regions (such as North America and Europe) than in tropical and southern climates. The “spared” zone is on the outskirts of the equator, between 40 ° north latitude and 40 ° south latitude. The reasons for this “gradient” are not yet known, but vitamin D (produced during exposure to the sun) may play a role.
People with an autoimmune thyroid problem, those with type 1 diabetes or inflammatory bowel disease are at slightly higher risk.
—
Multiple sclerosis risk factors
Studies of identical twins (who have the same hereditary background) reveal that environmental factors play a predominant role in the occurrence of the disease. Take the fictitious example of Julie and Sophie, real twins aged 30. Julie has had multiple sclerosis since she was 25 years old. Sophie’s risk of suffering from multiple sclerosis like her twin sister is estimated at 30%, while it should be 100% if the multiple sclerosis was of genetic origin alone. It is therefore mainly environmental factors that trigger the disease. This is probably a conjunction of many factors, not just one event.
The following risk factors are presented as assumptions:
Having a vitamin D deficiency. The distribution of multiple sclerosis cases around the world (more cases in less sunny countries) has led researchers to speculate a link between vitamin D and the risk of multiple sclerosis. This is because vitamin D is produced by the skin when exposed to the sun. Low sunlight, leading to vitamin D deficiency, could therefore be linked to the onset of the disease.
Several studies have evaluated the link between the level of vitamin D in the blood and the risk of multiple sclerosis. In 2004, a study of 2 cohorts with a total of 187,563 nurses found that women who took a daily vitamin D supplement (400 IU or more) reduced their risk of developing multiple sclerosis by 40%. In 2006, a study of American soldiers showed that those with the highest vitamin D levels had a lower risk of developing multiple sclerosis. In an article published in 2013, it is estimated that the risk of developing multiple sclerosis is reduced by 30% in women with the highest levels of vitamin D, compared to those with the lowest levels. Multiple sclerosis is not believed to be the first autoimmune disease associated with low vitamin D levels.
In addition, vitamin D levels are low in the majority of people with the disease, especially at the onset of the disease. Finally, studies in mice show that vitamin D may reduce the number of relapses and slow the progression of the disease19. Unfortunately, current data cannot determine whether vitamin D supplementation can influence disease progression in men.
Having contracted the Epstein-Barr virus. This virus, involved in infectious mononucleosis, has been implicated by several studies in the onset of the disease. However, no formal proof of his involvement could be provided. In June 2010, a study of 900 people showed that the risk of multiple sclerosis increases after infection with the Epstein-Barr virus (EBV). In 2006, the same researchers had shown that people with the disease have a higher than normal level of anti-EBV antibodies. Finally, a recent meta-analysis of 18 studies and over 19,000 people concluded that contracting infectious mononucleosis increases the risk of developing multiple sclerosis.
Smoke cigarettes. People who smoke 20 to 40 cigarettes a day are about twice as likely to have multiple sclerosis as non-smokers. In addition, smoking appears to worsen symptoms in sufferers and accelerate the progression from relapsing-remitting forms to progressive ones.
Consume lots of saturated fat, salt, and ultra-processed foods. Multiple sclerosis is thought to be more common in populations whose diets are rich in animal fats, industrial foods and salt and lower in those who consume mainly polyunsaturated fatty acids. Since northern populations generally eat a diet higher in animal fat, it is difficult to isolate the impact of diet from that of geographic location. As mentioned earlier, multiple sclerosis is 5 times more common in northern or temperate regions than in tropical and southern climates.
Being in contact with chemical solvents in the workplace35
Notes. There is evidence in the scientific literature that wearing mercury dental amalgam increases the risk of multiple sclerosis and also worsens its symptoms. However, the majority of these data come from studies whose scientific quality is considered to be low. Having had multiple mercury amalgams over the years could increase the risk of developing the disease, but this has not been clearly demonstrated. Thereby, doctors generally consider dental amalgams not to be a problem.
What is the cause of MS?
Multiple sclerosis is a disease with complex determinism involving genetic susceptibility factors and environmental factors.
Genetic susceptibility does not mean inherited disease. There are no genetic abnormalities in people with MS that are found in hereditary diseases, such as gene mutations that disrupt certain cellular functions responsible for these diseases. Genetic susceptibility means that individual variations (alleles) of certain completely normal genes can make them more vulnerable to certain environmental factors and help trigger disease in individuals who carry them. Research is focused on identifying these genes.
Epidemiology studies environmental factors. The MS is distributed according to a gradient of latitude. It is more frequent when one moves away from the equator and its prevalence increases as one goes up in latitude. Recent studies suggest that the amount of sunshine, possibly via the production of vitamin D, could be one of the important protective factors. The role of viruses is strongly suggested although no virus could be specifically associated with MS. The infectious mononucleosis virus (EBV virus) is particularly the subject of extensive research.
The gene-environment interaction helps trigger an abnormal reaction of the immune system by activating self-reactive lymphocytes with myelin components of the central nervous system. The successive reactivation phases at the origin of the outbreaks will amplify and transform an intermittent inflammation into a continuous inflammation involving other cellular actors. The latter is at the origin of the progressive degeneration of fibers and nerve cells.
Type of MS
Several typical patterns of symptoms:
1. Relapsing-remitting pattern: Relapses (when symptoms worsen) alternate with remissions (when symptoms lessen or do not worsen).
2. Remissions may last months or years. Relapses can occur spontaneously or can be triggered by an infection such as influenza.
3. Primary progressive pattern: The disease progresses gradually with no remissions or obvious relapses, although there may be temporary plateaus during which the disease does not progress.
4. Secondary progressive pattern: This pattern begins with relapses alternating with remissions (the relapsing-remission pattern), followed by gradual progression of the disease.
5. Progressive relapsing pattern: The disease progresses gradually, but progression is interrupted by sudden relapses. This pattern is rare.
On average, without treatment, people have about one relapse every 2 years, but frequency varies greatly.
Treatments and Medications
What are the treatments for MS?
It is usual to treat MS relapses with a short course of high doses of corticosteroids (eg methylprednisolone infusion 1g per day for 3 days).
Relapsing-remitting (relapsing) MS require treatments that reduce aggressive responses of the immune system. Immunomodulators (beta 1a or 1b interferons of which there are several presentations and routes of administration, glatiramer acetate) represent the first-line treatments. They are instituted early, when the diagnosis of the disease is assured. Second-line treatments or immunosuppressants (natalizumab, mitoxantrone) are available when the efficacy of immunomodulators is insufficient. They have a greater amplitude of effect, but at the expense of a higher level of therapeutic risk. Immunosuppressants in general increase the risk of infections, sometimes of hematological diseases, by reducing the body’s defenses.
Therapeutic research is very active. New drugs, easier to use, will be available soon. Like all immunosuppressive or immunomodulatory treatments, however, they have no efficacy on the progressive development of the handicap which characterizes the second phase of the disease. The inflammatory mechanism is in fact accompanied by a mechanism of degeneration of nerve fibers which currently remains untreated.
—
Multiple sclerosis medical treatments
There is no cure for multiple sclerosis, but medical research has found drugs that alleviate symptoms relatively effectively and that slow the progression of the disease and reduce the number and / or intensity of flare-ups. The earlier treatment is started, the better.
The neurologist specializing in the management of multiple sclerosis offers treatments depending on the course of the disease, but also their potential adverse effects. Do not hesitate to ask him questions or to tell him about a problem encountered.
Treatment of relapses
Flare-ups don’t necessarily need treatment, as they usually subside within a few days.
Corticosteroids are most often prescribed as an infusion (bolus) to reduce the duration of an attack and promote recovery. Side effects (insomnia, increased blood pressure, mood swings, fluid retention, osteoporosis) can be severe.
DMARDs
DMARDs reduce the frequency and intensity of relapses and therefore ultimately help slow the progression of the disease. They are usually offered upon diagnosis of relapsing-remitting multiple sclerosis and should be taken continuously, even if there are no symptoms.
There is a great deal of scientific data demonstrating the value of early treatment in reducing the frequency of relapses.
There are 2 types of DMARDs: immunomodulators and immunosuppressants. These treatments reduce the activity of the immune system, thus slowing down the destruction of myelin.
Immunomodulators
They include molecules from the beta interferon family: they are taken by injection (subcutaneously or intramuscularly).
Interferons are substances produced naturally by the body to inhibit the multiplication of viruses and stimulate the activity of certain immune cells. They reduce the frequency of relapses by about 30%. However, they often cause a flu-like syndrome (fever, chills, headache, muscle pain) and skin reactions a few hours after the injection during the first 3 months of treatment. These side effects go away afterwards. Liver damage (reversible) is common, but usually mild. Patients then need to do blood tests to monitor their liver enzymes. People taking interferons can also develop neutralizing antibodies which can reduce the effectiveness of the medicine.
Your doctor may also prescribe glatiramer acetate (Copaxone®), another immunomodulator. As with interferons, injections can cause local inflammatory reactions (redness, pain, etc.). Headaches, anxiety, flushing, palpitations and infections are among the most commonly reported side effects.
Dimethyl fumarate (Tecfidera®) is a medicine taken by mouth twice a day and indicated for the treatment of patients with relapsing-remitting multiple sclerosis. It appears to reduce relapses, with side effects including diarrhea, nausea, and reduced numbers of certain white blood cells, hence the need for blood cell monitoring.
Teriflunomide (Aubagio®) is a drug that can reduce the rate of relapse. However, it can cause liver, hematological and skin damage. It is harmful to the fetus and therefore should not be used in women who want to become pregnant and / or pregnant.
Immunosuppressants
Mitoxantrone, also administered as an infusion, is a treatment used in certain cancers, but which has shown an interest in multiple sclerosis of rapid progression, disabling and which does not respond to other treatments.
Natazilumab is a monoclonal antibody, given as an infusion, reserved for very active forms of multiple sclerosis. It is reserved for patients whose condition does not improve with other treatments or who cannot tolerate them or for people with severe multiple sclerosis. Natalizumab increases the risk of progressive multifocal leukoencephalopathy, a rare brain condition caused by a virus and which can be fatal. It can also be toxic to the liver.
Ocrelizumab (Ocrevus®) is indicated for early stage disease and disability because clinical trials have failed.
It was found to modestly reduce disease progression in the primary progressive form. Ocrevus also helps reduce relapses in the relapsing-remitting form. Ocrevus, which is given as an infusion, can cause side effects such as irritation at the injection site and most importantly, promote upper respiratory infections. Ocrevus may also increase the risk of certain cancers, including breast cancer.
Fingolimod (Gilenya®) was approved in September 2010 by the FDA health agency in the United States and in March 2011 by Health Canada. This medicine has the advantage of being taken by mouth. It would reduce the frequency of relapsing-remitting multiple sclerosis and slow the progression of the disease. The heart rate should be monitored for six hours after the first dose, since taking the medicine is usually accompanied by a decrease in heart rate. Side effects include headaches and blurred vision. They are reserved for more severe multiple sclerosis. More powerful than immunomodulators, they require special monitoring because the risk of infection is particularly increased.This treatment requires cardiac monitoring and monitoring of blood cells. Its use in the treatment of multiple sclerosis is extremely limited. Mitoxantrone is usually only used to treat severe and advanced multiple sclerosis.
Another orally administered drug already used to combat certain forms of leukemia – cladribine – received encouraging results published in 2017 (American Academy of Neurology Annual Meeting, Boston, USA). A subgroup of patients with a higher risk of disease progression experienced, on cladribine, a greater than 80% reduction in the risk of disability progression, compared to the placebo group. Cases of progressive multifocal leukoencephalopathy have also been reported with this treatment.
Other drugs exist such as alemtuzumab (Lemtrada®) but the High Authority of Health considers that it presents a moderate improvement in actual benefit only in severe forms, defined by at least two debilitating attacks during one. year.
Relief treatments for MS
There are several drugs and treatments that can be used to relieve many symptoms, including fatigue, muscle spasms, pain, sexual dysfunction, and urinary tract problems. Here are a few.
Physiotherapy and rehabilitation. These are important parts of the care. The goal of rehabilitation is to preserve certain functions (such as walking), to reduce complications (urinary disorders, spasms) and to learn how to live with a disability as well as possible. If necessary, the physiotherapist or occupational therapist can suggest and adapt technical aids (cane, wheelchair, etc.) to make daily life easier.
Against pain. Neurontin® (an anticonvulsant) and Elavil® (a tricyclic antidepressant) are usually effective. Sativex®, (therapeutic cannabis), can also be used (in the form of a spray directed under the tongue or on the inside of the cheek): it has been authorized in France since 2014 in theory, but cannot be found in pharmacies for lack of agreement. on its price between the laboratory and the health authorities (a solution is expected before the end of 2019). Paracetamol and ibuprofen, available over the counter, may help occasionally.
Against muscle spasms. Muscle relaxants and stretching exercises help reduce leg spasms, which can be painful.
Against fatigue. Fatigue is extremely common in people with multiple sclerosis and can significantly affect quality of life. In addition to adapting your daily life to your state of fatigue, it is possible to take certain prescription drugs indicated for other illnesses.
Against urinary problems. Several drugs can be prescribed to increase the muscle strength of the bladder or sphincter and limit leakage.
Canadians with multiple sclerosis can use smoked marijuana to relieve acute pain and persistent spasms, as specified in the Access to Medical Marijuana Regulations. For more information, visit Health Canada’s Marijuana Medical Access Division web page (Sites of Interest section).
Oxygen treatment in a hyperbaric chamber. This treatment consists of inhaling, in a chamber, pure oxygen at a pressure higher than normal. It was tested intensively in England from 1983 to 1987. Many patients have reported benefiting from it, the treatment mainly seeming to improve bladder and bowel functions. However, none of the double-blind, controlled studies in this area have shown a positive effect on the objective endpoints of the disease. For this reason, Health Canada does not approve the use of this therapy for multiple sclerosis. It is not offered in France either.
What is magnetic resonance imaging (MRI) used for in the diagnosis and monitoring of MS?
MRI is a very useful brain and spinal cord imaging technique for visualizing inflammatory lesions in MS. The abnormal images result in easily identified changes in the MRI signal of normal nerve tissue. Various analysis sequences make it possible to quantify the lesions, to identify their recent nature when they are enhanced by a contrast product injected by the intravenous route (gadolinium), and to assess their concordance with the diagnosis of MS. Indeed, the images are not specific to the disease and must be analyzed in the light of the information collected by clinical and biological examinations.
The systematic repetition of MRI examinations during the course of the disease is not useful. The neurologist can use MRI when he is uncertain about the therapeutic efficacy or when changing treatment. The conventional MRI outside of research shows only a small part of the lesions which does not make it a very reliable tool in the assessment of the handicap and its evolution. It is seldom used during the progressive phases of MS.
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Mayo Clinic, NHS (UK), Healthline, Web MD, The Johns Hopkins University
Photo credit: Mikael Häggström / Wikimedia Commons