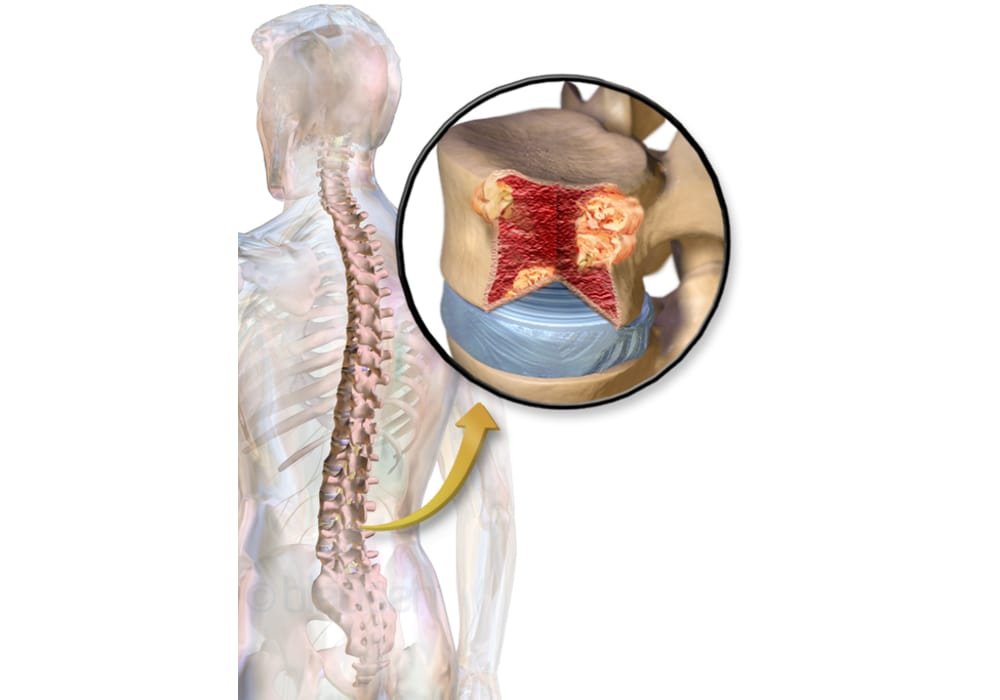
Multiple Myeloma
Multiple Myeloma or briefly Myeloma is cancer that starts in plasma cells. Plasma cells are a type of white blood cell that make antibodies (immunoglobulins) to help fight infections. This is a type of bone marrow cancer. Bone marrow is the spongy tissue at the centre of some bones that produces the body’s blood cells.
Plasma cells are found primarily in the bone marrow, but they are also found in some other tissues and organs. Bone marrow is the soft, spongy tissue that occupies the interior of most bones, where different types of blood cells are made. The plasma cells in the bone marrow sometimes undergo changes that make the way they grow or behave abnormally. These abnormal plasma cells start to proliferate in a disorderly fashion and produce other abnormal plasma cells. These changes can lead to multiple myeloma (cancer of the plasma cells) or a precancerous condition called monoclonal gammopathy of undetermined significance (MGUS). Precancerous means that the cells are not yet cancerous, but have a higher risk of becoming cancerous. In some cases, MGUS can progress to multiple myeloma.
Multiple myeloma occurs when there is a buildup of many abnormal plasma cells (myeloma cells) in the bone marrow. This prevents other blood cells in the marrow from growing normally and doing their usual jobs. The buildup of myeloma cells can cause anemia and fatigue because there are fewer red blood cells. It can also upset the balance of certain minerals in the body. Myeloma cells make a substance that can cause bone damage and increase calcium levels in the blood. They also produce abnormal proteins that can affect other organs, such as the kidneys.
Myeloma cells can form tumors in the bones called plasmacytomas. We talk about a solitary plasmacytoma when there is only one tumor in a bone. When there are a lot of plasmacytomas in the bones, the disease is called multiple myeloma. Plasmacytomas can also form outside of the bones. These tumors are called extramedullary plasmacytomas.
Types of multiple myeloma
Multiple myeloma is the most common type of malignant plasma cell proliferation. It is mainly in the bones and bone marrow that myeloma cells (abnormal plasma cells) are produced. Myeloma cells can form tumors, called plasmacytomas, in many bones of the body.
The accumulation of myeloma cells causes:
- a decrease in the number of normal blood cells in the bone marrow;
- weakening or deterioration (fracture) of bones;
- bone pain;
- an infection.
When the bones are weakened or damaged, it is a sign that 2 types of bone cells no longer work together as they usually do. Osteoblasts make up bones and osteoclasts break down bones. Myeloma cells stimulate osteoclasts, which break down bones at a much faster rate than normal.
Main Types
There are 2 main types of multiple myeloma: latent multiple myeloma and active multiple myeloma. Latent multiple myeloma does not cause signs and symptoms. Active multiple myeloma causes signs and symptoms.
1. Latent multiple myeloma (indolent)
Latent (indolent) multiple myeloma is also called asymptomatic myeloma because it does not cause symptoms at all. This type of myeloma falls between monoclonal gammopathy of undetermined significance (MGUS, a precancerous condition) and active multiple myeloma (symptomatic). People with latent multiple myeloma have at least one of the following characteristics.
Plasma cells make up 10% or more of the blood cells in the bone marrow.
The level of M protein in the blood is at least 30 g / L. An M protein is a type of immunoglobulin that is produced by abnormal plasma cells.
Most people with latent multiple myeloma will one day have multiple myeloma with symptoms (active multiple myeloma).
People with latent multiple myeloma have the usual tests every 3 to 6 months to see if the disease progresses to active multiple myeloma. Only people with very high risk latent multiple myeloma can be treated.
Risk categories
Doctors are trying to predict when people with latent multiple myeloma will have active multiple myeloma.
Low risk latent multiple myeloma
You have low-risk latent multiple myeloma if you have both of the following characteristics:
Plasma cells make up less than 10% of blood cells in the bone marrow.
The level of M protein in the blood is at least 30 g / L.
On average, low-risk latent multiple myeloma progresses to active multiple myeloma about 19 years after diagnosis.
Medium risk latent multiple myeloma
You have medium risk latent multiple myeloma if you have both of the following characteristics:
Plasma cells make up 10% or more of the blood cells in the bone marrow.
The level of M protein in the blood is less than 30 g / l.
On average, medium-risk latent multiple myeloma progresses to active multiple myeloma about 9 years after diagnosis.
High risk latent multiple myeloma
You have high-risk latent multiple myeloma if you have both of the following characteristics:
plasma cells constitute at least 10% of blood cells in the bone marrow;
the level of M protein in the blood is at least 30 g / l.
On average, high-risk latent multiple myeloma progresses to active multiple myeloma approximately 2.5 years after diagnosis.
In some cases, high risk latent multiple myeloma is at very high risk of developing to active multiple myeloma within 2 years of diagnosis if all of the following are present:
plasma cells make up at least 60% of the blood cells in the bone marrow;
the level of serum free light chains is at least 100;
an MRI shows more than one region of bone or bone marrow destruction (breakdown).
If you have this type of high-risk latent multiple myeloma, you will be treated as if you have stage 1 multiple myeloma.
2. Active multiple myeloma (symptomatic)
People with multiple myeloma who have symptoms of the disease and any of the following have active (symptomatic) multiple myeloma:
M protein in the blood or urine
Plasma cells which make up 10% or more of the blood cells in the bone marrow
Tumor that contains myeloma cells (plasmacytoma) in bone or soft tissue
Anemia, kidney failure or high blood calcium (hypercalcaemia)
Osteolytic lesions (weakened areas of the bone, which can be seen on an x-ray)
3. Solitary bone plasmacytoma
A plasmacytoma occurs when abnormal plasma cells accumulate in the same location and form a single tumor. Solitary bone plasmacytoma is a single tumor made up of myeloma cells that occurs in a single bone (rather than multiple tumors, or more than one tumor, seen in different places, as in multiple myeloma). It does not have other characteristics of multiple myeloma. The bone x-ray shows only an osteolytic lesion at the site of the plasmacytoma, and plasma cells make up less than 10% of all cells in the bone marrow. The main symptom of a solitary bone plasmacytoma is pain at the location of the tumor. A solitary plasmacytoma is most often treated with radiation therapy.
About a third of people with a solitary plasmacytoma will eventually develop other plasmacytomas and multiple myeloma.
4. Extramedullary plasmacytoma
Extramedullary plasmacytomas start outside the bone marrow (extramedullary) in soft tissue. It most often affects areas of the upper respiratory tract, such as the throat, the sinuses that surround the nose (paranasal sinuses), the nasal cavity, and the larynx (organ of speech). It can also develop in other areas, including the digestive tract, breasts and brain. Extramedullary plasmacytoma is diagnosed after biopsy of the tumor. In people with extramedullary plasmacytoma, x-rays and bone marrow biopsies are normal. An MRI or a PET may be done to look for other areas of the body that might show signs of cancer.
The main treatment for extramedullary plasmacytoma is radiation therapy, surgery, or both.
5. Light chain myeloma
In some people with multiple myeloma, myeloma cells do not make complete immunoglobulin. In people with light chain myeloma, only the light chain part of the immunoglobulin is produced and not the heavy chain part.
Light chains can build up in the kidneys and damage them. Light chains are smaller than M proteins and are more visible in urine than in blood: this is because the light chains have already been cleared from the blood when they reach the kidneys. The light chains found in urine are also called Bence-Jones proteins. In about 15% to 20% of people with multiple myeloma, the myeloma is light chain.
6. Non-secreting myeloma
In some people with multiple myeloma, myeloma cells do not release (secrete) enough M proteins or light chains in the blood or urine to be detected by protein electrophoresis. In non-secreting myeloma, there are myeloma cells in the bone marrow. X-rays also show osteolytic lesions in a person with non-secreting myeloma.
7. Rare types of multiple myeloma
The immunoglobulins (Ig) most often made by myeloma cells in the presence of multiple myeloma are IgG and IgA. The least common are IgD and IgE.
Immunoglobulin D (IgD) myeloma
In about 2% of people, multiple myeloma is of the IgD type. IgD multiple myeloma has the same signs and symptoms as other types of multiple myeloma. IgD myeloma tends to affect people who are a little younger, on average around 54 years old.
Immunoglobulin E (IgE) myeloma
IgE is the rarest type of multiple myeloma. IgE multiple myeloma has the same signs and symptoms as other types of multiple myeloma. It tends to be aggressive and develops into plasma cell leukemia or spreads rapidly outside the bone marrow.
Enzymes in the Digestive System – How Enzymes Work: Definition and Examples
Risk factors for multiple myeloma
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors, but sometimes multiple myeloma develops in people who do not have any of the risk factors described below.
More men than women are diagnosed with multiple myeloma. The risk of getting this disease increases with age. People of African descent are at greater risk of developing multiple myeloma. We do not know the reasons for this increased risk.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
History of monoclonal gammopathy of undetermined significance (MGUS)
MGUS is a plasma cell disorder that can develop into multiple myeloma. A plasma cell is a type of white blood cell that makes antibodies to help the body fight infections. Many known and possible risk factors for MGUS are the same as those for multiple myeloma.
It is difficult to diagnose multiple myeloma in its early stages. Often, symptoms do not appear until the disease is more advanced. People with MGUS may have to have regular blood tests to make sure their condition does not progress to multiple myeloma.
Family history of multiple myeloma
Multiple myeloma is more common in some families. The risk of being affected is almost 4 times higher for a person whose mother or father or a brother or sister suffers from it. Some studies show that the risk is greater in families of African descent. But most people with multiple myeloma do not have a family history of the disease.
Obesity and overweight
Multiple myeloma more often affects people who have a body mass index (BMI) higher than those at a healthy weight.
Agricultural work
Many studies show that people who work in agriculture are more likely to have multiple myeloma. More research is needed to understand how agricultural work increases this risk. Some studies suggest that exposure to certain pesticides used in agriculture explains the increased risk. Pesticides contain a lot of different chemicals, but only a few of them are associated with the risk of multiple myeloma. Research also shows that people who work with farm animals, especially sheep, may be at increased risk. It is possible that a combination of several factors – exposure to pesticides, working with animals or other factors – may increase the likelihood of having multiple myeloma.
Weakened immune system
People with weakened immune systems (immunosuppression) have a higher risk of developing multiple myeloma. This includes people with HIV or AIDS, as well as those who have had an organ transplant and need to take medicines to weaken their immune systems.
Possible risk factors
The following factors have been linked to multiple myeloma in some way, but there is insufficient evidence to suggest that they are risk factors. More research is needed to clarify the role of these factors in the development of multiple myeloma:
- autoimmune disorders
- some viral infections like hepatitis B and hepatitis C
- work activities in fields such as oil production, machinery production or carpentry, where workers are exposed to chemicals such as benzene, coal or wood dust
Symptoms of multiple myeloma
Multiple myeloma may not cause any signs or symptoms in the early stages of the disease. Signs and symptoms often appear after the tumor has grown in the bone marrow or somewhere outside the bone marrow. Signs and symptoms may also occur if immunoglobulins (M proteins) build up in organs such as the kidney.
Other medical conditions can cause the same signs and symptoms as multiple myeloma. See your doctor if you have the following signs or symptoms:
- bone pain related to a bone fracture that has most often occurred in the back, front of the chest, ribs, hips or skull;
- bone weakness, which can lead to osteoporosis (a condition characterized by loss of bone mass, or density, and breakdown of bone tissue);
- fatigue, weakness, shortness of breath, dizziness and pallor caused by a low number of red blood cells (anemia);
- frequent infections, including pneumonia (infection of the lung), linked to a reduction in the number of white blood cells (neutropenia);
- fever (related to infection);
bleeding from the nose or gums, heavy bleeding from minor cuts or scrapes, or having a lot of bruising related to a reduced number of platelets (thrombocytopenia);
higher than normal level of protein in the blood or urine; - excessive thirst, need to urinate often, dehydration, kidney problems including kidney failure, constipation, loss of appetite, abdominal pain, weakness, drowsiness, confusion, nausea and vomiting or lethargy caused by high levels of calcium in the blood (hypercalcemia );
nervous system disorders including sudden severe pain, numbness and tingling, muscle weakness, paralysis, confusion and dizziness – some of these symptoms may be related to spinal cord compression, which is an emergency due to cancer; - weightloss;
- headache, dizziness, weakness, drowsiness, fatigue, oozing from cuts, slightly blurred vision, bruising, symptoms of a stroke (weakness on one side of the body and slurred speech) caused by hyperviscosity of the blood, either blood that has become thicker or stickier than usual;
- weakness, shortness of breath, itching and swelling caused by kidney problems.
Some of the more common signs and symptoms of multiple myeloma are referred to as “CRAB”:
- high level of calcium in the blood (hypercalcaemia);
- kidney problems (renal failure);
- anemia;
- bone disease.
Diagnose multiple myeloma
The diagnostic process for multiple myeloma usually begins with a visit to your family doctor. Your doctor will ask you about your symptoms and do a physical exam. Based on this information, your doctor may refer you to a specialist or order tests to check for multiple myeloma or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay to worry, but try to remember that other medical conditions can cause symptoms similar to multiple myeloma. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of multiple myeloma.
The following tests are commonly used to rule out or diagnose multiple myeloma. Many tests that can diagnose cancer are also used to determine its stage, that is, how far the disease has progressed. Your doctor may also give you other tests to check your general health and help plan your treatment.
Health history and physical examination
Your health history consists of a checkup of your symptoms, risk factors, and any medical events and conditions you may have had in the past. Your doctor will ask you questions about your history:
- symptoms that suggest multiple myeloma;
- abnormal blood test or urine test results.
Your doctor may also ask you questions about your family history of blood-related conditions, including multiple myeloma.
The physical exam allows the doctor to look for any signs of multiple myeloma.
Complete blood count
The complete blood count (FSC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. Myeloma cells (abnormal plasma cells) prevent these normal blood cells from growing in the bone marrow. FSC is used to find out if there are too few of these cells in the blood, which can lead to:
- anemia (low number of red blood cells);
- bleeding disorders (caused by a low number of platelets);
- a weakened immune system and infections (caused by a low number of white blood cells).
Blood biochemical analyzes
A blood chemistry test measures the level of chemicals in the blood. It makes it possible to assess the quality of functioning of certain organs and also to detect anomalies. The following chemicals may be found in abnormal amounts in people with multiple myeloma:
- proteins;
- creatinine;
- albumin;
- calcium;
- alkaline phosphatase;
- Uric acid;
- beta 2-microglobulin;
- lacticodehydrogenase (LDH).
Immunoglobulin (Ig) assay
The immunoglobulin (Ig) assay allows you to measure the amount of different antibodies
(special types of protein molecules also called immunoglobulins) in the blood to see if their numbers are high or low. There are 5 types of immunoglobulins – IgA, IgD, IgE, IgG and IgM. One of these antibodies is often seen to increase in the presence of multiple myeloma. IgG and IgA are the immunoglobulins most often found in large amounts in people with multiple myeloma.
Protein electrophoresis
Protein electrophoresis is a method that separates proteins from blood or urine. It is a test that is used to find out if:
- proteins are abnormal;
- proteins are absent;
- protein levels are too high or too low.
In people with multiple myeloma, 70% have high levels of the protein called IgG, 20% have high IgA levels, and 5-10% only produce light chains of immunoglobulins (Bence-Jones proteins).
Serum protein electrophoresis
Electrophoresis of serum proteins makes it possible to verify the presence of the M protein in the blood. M protein is an immunoglobulin produced in large quantities in a person with multiple myeloma.
Urinary protein electrophoresis
Urinary protein electrophoresis checks for the presence of M protein in urine that has been collected over a 24 hour period. Urinary protein electrophoresis can also detect a part of the M protein called the immunoglobulin light chain (also called the free light chain or Bence-Jones protein).
Immunofixation
Immunofixation is a specialized type of electrophoresis that identifies the type of M protein or immunoglobulin light chain that has been detected by electrophoresis of serum or urine proteins.
Determination of serum free light chains
The serum free light chain assay can detect immunoglobulin light chains (called free light chains or Bence-Jones proteins) in the blood. This test can be useful in diagnosing multiple myeloma if the M protein is not detected by serum protein electrophoresis.
The assay of free serum light chains also makes it possible to measure the level of light chains. The level of light chains indicates if there is an imbalance between the amounts of each light chain, which may be a sign of multiple myeloma. Immunoglobulins have 2 types of light chains: kappa, lambda. About the same amount of each of these free light chains is found.
Urine analysis
Urinalysis is a common urine test that determines the color, appearance and contents of a urine sample. It can be used to measure the amount of protein in urine.
The doctor will normally ask you to collect your urine over a 24 hour period. Urinary protein electrophoresis can be used to check for the presence of Bence-Jones proteins in the sample. High levels of Bence-Jones protein could damage the kidneys.
Biopsy
During a biopsy, the doctor removes tissues or cells from the body for analysis in the laboratory. The pathology report from the laboratory will confirm the presence of cancer cells in the sample.
The most common type of tissue biopsy done to diagnose multiple myeloma is a bone marrow biopsy and puncture. The doctor may also do a biopsy to check for the presence of amyloid if he is having difficulty making a diagnosis of multiple myeloma.
Bone marrow puncture and biopsy
A bone marrow biopsy and puncture takes cells from the bone marrow for examination under a microscope. The pathology report from the laboratory will confirm the presence of abnormal plasma cells in the sample. The report will also show the percentage of plasma cells in all cells of the bone marrow.
Tissues collected during the bone marrow puncture and biopsy can be used for other tests such as cytogenetics, immunohistochemistry and flow cytometry.
Biopsy to check for the presence of amyloid substance
Amyloid refers to a protein or part of a protein that forms abnormal clumps in the body. In light chain amyloidosis, the light chains of an immunoglobulin build up in body tissues (amyloid deposits). Amyloid can build up in any tissue and interfere with proper function. Light chain amyloidosis is a condition that can affect people with multiple myeloma.
Sometimes amyloid is found during a bone marrow biopsy, but the doctor may remove other tissue, such as fatty tissue from the abdomen (tummy), to check if amyloid is present. In rare cases, the doctor will take a heart or kidney biopsy to check for the presence of amyloid. This is done only if it is not known exactly why the person is having heart or kidney problems.
Other tissue biopsies
Doctors may also take a biopsy of other suspicious areas of the body, including:
an abnormal bone area seen on x-ray – to check for the presence of plasmacytomas;
a tumor on the outside of the bone – to check for the presence of extramedullary plasmacytomas.
Cytogenetic tests
Cytogenetics is the study of a cell’s chromosomes, including their number, size, shape and arrangement. Cytogenetic tests (analysis of chromosomes) reveal the chromosomal changes that affect some people with multiple myeloma. The results of cytogenetic studies also help doctors plan treatment and predict its effectiveness.
Cytogenetic tests that are used in people with multiple myeloma include karyotyping and fluorescence in situ hybridization (FISH).
Karyotyping
The doctor checks the cells for chromosomal changes from a blood or bone marrow sample. Karyotyping can detect large chromosome changes, such as missing part of a chromosome or missing an entire chromosome. Chromosome 13 is sometimes missing (deletion) in people with multiple myeloma. Karyotyping can also detect small chromosomal changes, such as rearrangement of a chromosome. Chromosome 14 is commonly rearranged (translocated) in people with multiple myeloma. It may take up to 2 or 3 weeks for karyotyping results to be known since cells must be allowed to grow in the lab before testing.
Fluorescence in situ hybridization (FISH)
Significant chromosomal changes can be detected by looking at cells under a microscope. But most changes in DNA need to be analyzed more carefully using other molecular techniques. Fluorescence in situ hybridization (FISH) is a special molecular genetic test used to detect chromosomal changes and other genetic changes in cells using special DNA probes labeled with fluorescent dyes. FISH can detect small chromosome changes, such as a rearrangement or missing chromosome. It only takes a few days to get the FISH results since you do not need to let the cells grow in the lab before testing.
Immunohistochemistry
Immunohistochemistry is a test in which special staining is used to check the details of a cell. Immunohistochemistry can help check for the presence of specific proteins that are often found in people with multiple myeloma. This gives the doctor more information than the dye tests usually used to check the size and shape of cells.
Flow cytometry
Flow cytometry is a laboratory test that sorts, counts, and examines microscopic particles, such as cells or DNA. Cells are measured by adding a light-sensitive dye that binds to antibodies, then placing them in a liquid that is passed under a laser beam. The laser causes cells to emit light which is measured and analyzed by a computer. It quickly collects data on thousands of cells present in a single sample.
Flow cytometry can help doctors tell the difference between abnormal plasma cells (myeloma cells) and normal plasma cells.
X-ray
In an x-ray, low-dose radiation is used to produce images of body structures on film. Most bones in the body are examined on an x-ray to diagnose multiple myeloma. This is called a skeletal examination. Radiography is used to:
- check for broken or weakened bones in the skull, spine, legs, arms, ribs and pelvis;
- check for areas of bone that might indicate the presence of a plasmacytoma (a collection of
- myeloma cells in one place that forms a single tumor);
- measure bone loss (bone mineral content).
Find out more about x-rays.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) uses powerful magnetic forces and radio waves to produce cross-sectional images of the body’s organs, tissues, bones, and blood vessels. A computer assembles the images into 3-dimensional snapshots. MRI is used to:
- check for changes in the bone marrow;
- check for broken or weakened bones;
- detect the presence of plasmacytomas;
- check for compression of the spinal cord.
Find out more about MRI.
MRI guided fine needle biopsy
MRI may also be used to guide a needle during a fine needle biopsy (BAF) of a mass believed to be a plasmacytoma. Cytogenetic tests can then be done on the cells removed.
CT scan
A computed tomography (CT) scan uses special x-ray machines to produce 3-dimensional and cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the photos into detailed images. CT is used to:
- check for broken or weakened bones;
- detect the presence of a plasmacytoma.
CT guided fine needle biopsy
CT may also be used to guide a needle during a fine needle biopsy of a mass believed to be a plasmacytoma. Cytogenetic tests can then be done on the cells removed.
Positron emission tomography
A positron emission tomography (PET) scan uses a radioactive material called a radiopharmaceutical to detect changes in the metabolic activity of body tissues. Computer analyzes patterns of radioactivity distribution and produces 3-dimensional images ions and color of the examined region. PET is sometimes used to:
- check for changes in the bone marrow;
- detect the presence of a plasmacytoma.
PET / CT
A PET / CT combines a CT scan with a positron emission tomography. PET / CT is sometimes used to:
- know if there are any bones that are likely to fracture in people with normal x-rays;
- check for the presence of plasmacytomas inside and outside the bones.
Stages of multiple myeloma
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. The information from the tests is used to find out how big the tumor is, if the cancer has spread from where it started and where it has spread. When diagnosed, multiple myeloma is usually generalized. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The staging of multiple myeloma is based on the results of blood tests and imaging tests. The results of other tests can also help determine the stage depending on the system used.
Doctors use 2 systems to determine the stage of multiple myeloma:
International Staging System (ISS);
classification of Durie and Salmon.
In Canada, the stage of multiple myeloma is most commonly established using the International Staging System.
Grouping of stages for multiple myeloma
In the case of multiple myeloma, there are 3 stages. For stages 1 to 3, the Roman numerals I, II and III are often used. In general, the higher the number, the more cancer is present in the body. Talk to your doctor if you have any questions about the stage.
International Staging System
The International Staging System is based on the results of 2 blood tests to establish the stage of multiple myeloma, namely the level of albumin and the level of beta 2-microglobulin.
Albumin is the main protein found in plasma
It helps maintain blood volume. Beta 2-microglobulin is a protein found on the surface of cells that is released into the blood. It plays a role in the immune response
Stage 1
The beta 2-microglobulin level is less than 3.5 mg / l.
The albumin level is equivalent to or greater than 35 g / l.
Stage 2
The beta 2-microglobulin level is less than 3.5 mg / l.
The albumin level is less than 35 g / l.
WHERE
The level of beta 2-microglobulin is greater than 3.5 mg / L but less than 5.5 mg / L and the level of albumin can be any.
Stage 3
The level of beta 2-microglobulin is equal to or greater than 5.5 mg / L and the level of albumin can be any.
Classification of Durie and Salmon
The Durie and Salmon classification is based on the results of blood tests, urine tests and x-rays to determine the stage of multiple myeloma. The Durie and Salmon classification is based on the following factors:
amount of hemoglobin
in the blood;
amount of calcium in the blood;
number of bone lesions seen on x-ray;
amount of monoclonal proteins (M proteins) in the blood or urine (as IgG, IgA and free light chains).
Stage 1
There is a small amount of myeloma cells.
All of the following features are present:
the hemoglobin level is equivalent or greater than 100 g / l;
the blood calcium level is normal (less than 2.8 mmol / l);
there are no damaged bony areas or there is a solitary bone plasmacytoma;
the level of IgG is less than 50 g / l;
the level of IgA is less than 30 g / l;
urine M protein level is less than 4 g (24 hour urine collection).
Stage 2
There is a moderate amount of myeloma cells.
The characteristics vary between those of stage 1 and those of stage 3.
Stage 3
There is a large amount of myeloma cells.
One or more of the following characteristics are present:
The hemoglobin level is less than 85 g / l.
The blood calcium level is greater than 2.8 mmol / l.
There are several damaged areas of bone.
The IgG level is over 70 g / l.
The level of IgA is greater than 50 g / l.
Urinary M protein level is greater than 12 g (24 hour urine collection).
Substages of the Durie and Salmon classification
The stages of multiple myeloma are further divided according to the level of creatinine in the blood, which shows how well the kidneys are functioning.
Substage A
The kidneys are functioning normally. The creatinine level is less than 180 µmol / l.
Substage B
The kidneys are not functioning normally. The creatinine level is equal to or greater than 180 µmol / l.
Multiple myeloma recurrence
When multiple myeloma comes back, the cancer comes back after treatment. It can come back in the same place as the original myeloma or in another part of the body.
Spread of multiple myeloma
Multiple myeloma is usually generalized when diagnosed. It affects many (more than 1) bones or several regions of the same bone.
Multiple myeloma most commonly occurs in the following bones:
- spine (vertebra);
- ribs;
- sternum;
- hip;
- scapula (scapula);
- skull;
- arm bones (humerus);
- upper leg bone (femur).
Doctors measure substances in the blood or urine to see if the disease is progressing, or getting worse. They measure the levels of the following substances:
- hemoglobin;
- calcium;
- monoclonal protein (M protein);
- creatinine;
- beta 2-microglobulin.
Prognosis and survival for multiple myeloma
If you have multiple myeloma, you may have questions about your prognosis. Prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type, stage and characteristics of the cancer you have, the treatments chosen and the response to treatment can look at all of this data together with survival statistics to come to a conclusion. prognosis.
A prognostic factor is an aspect of cancer or a characteristic of the person that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. We often discuss prognostic and predictive factors together. They both play a role in choosing the treatment plan and in establishing the prognosis.
The following are the prognostic factors and predictors of multiple myeloma
Stadium
People with early stage multiple myeloma usually have a better prognosis.
Age
Young people have a better prognosis than older people.
Blood test results
The results of some blood tests are important in determining the prognosis in people with multiple myeloma.
Beta 2-microglobulin
Beta 2-microglobulin is a protein found on the surface of myeloma cells, which participates in the immune response. A high level of beta 2-microglobulin leads to a poor prognosis. The level of this protein increases if:
- the number of myeloma cells increases;
- the kidneys are damaged.
Albumin
Albumin is the main protein in plasma
which helps maintain blood volume. A high level of albumin leads to a better prognosis.
Lacticodehydrogenase
Lacticodehydrogenase (LDH) levels are measured to understand the extent of cancer in the body (tumor burden). A high level of LDH has a poorer prognosis.
Creatinine
Creatinine is a breakdown product made in muscles and released from the blood by the kidneys. Measuring the level of creatinine in the blood shows how well the kidneys are functioning. People with multiple myeloma who have high creatinine levels have a poorer prognosis.
Chromosome changes
Doctors examine cells taken from the bone marrow to see if there are any changes to the chromosomes. Some chromosome changes are linked to a poorer prognosis, including the following:
Absence of chromosome 13 (deletion)
Lack of part of chromosome 17 (deletion 17p)
Shifting of chromosome 14 (translocation)
Additional copy of part of chromosome 1 (gain or amplification)
Risk stratification based on chromosome changes
Doctors can predict which people with multiple myeloma are most likely to have the best or worst prognosis based on the number and type of chromosomal changes. This is called risk stratification. People will be told if they are at good (low), medium, or high risk.
Good (low) risk – the person is likely to survive for 8-10 years
Medium risk – the person is likely to survive for 5 years
High risk – the person is likely to survive for less than 2 years
Kidney function
People whose kidneys are not functioning well have a poor prognosis. Doctors can measure the level of creatinine in the blood to check how well the kidneys are working.
Dialysis can help improve kidney function in people with multiple myeloma.
Percentage of plasma cells in S phase
The percentage of S-phase plasma cells is a measure of how fast myeloma cells are growing in a sample of cells taken from the bone marrow. A high percentage of S phase plasma cells indicates that myeloma cells will grow rapidly and is linked to a poor prognosis.
Functional index
The Functional Index is on a scale of 0 to 4. A low number indicates that the person is healthier and able to be more active than someone with a high Functional Index. The functional index is important in multiple myeloma because people with a good functional index are able to endure intensive treatments which may have a better prognosis, but have more side effects.
Response to treatment
People whose cancer responds well to treatment and who achieve complete remission have a better prognosis than this.
They whose cancer does not respond to the initial treatment.
Genetic signatures
The gene expression profile is a way for doctors to analyze many genes at once to find out which are active and which are not. Doctors have found several abnormal genetic patterns (genetic signatures) in people with multiple myeloma. These genetic signatures help to establish a prognosis. Some genetic signatures are associated with a better prognosis and better response to treatment, while other signatures are associated with a poorer prognosis.
Treatments for multiple myeloma
If you have multiple myeloma, your healthcare team will create a treatment plan just for you. It will be based on your condition and specific cancer information. When your healthcare team decides which treatments to offer you for multiple myeloma, they will consider the following:
your age and state of health;
if you have any symptoms, and which ones;
if there are any complications from the disease, such as poor functioning of the kidneys;
if you are eligible for a stem cell transplant – it depends on age, functional index
and the presence of other health problems;
risk stratification based on chromosome changes – you will be told whether you are good (low), medium or high risk;
the type of multiple myeloma;
the stage of multiple myeloma;
if you have received any other treatment and how you reacted to the treatment;
if you are a good candidate to participate in a clinical trial.
Multiple myeloma cannot be cured. The aim of treatment is to reduce symptoms, slow the progression (progression) of the disease and bring the disease into remission. Remission for multiple myeloma is achieved when most or all of the signs and symptoms of the disease are gone.
Response to treatment
At some point after your treatment, you will have tests that will help the doctors know how well the treatment is working. This is called the reaction to treatment. The International Myeloma Working Group categorizes the response to treatment into the following categories:
Strict full response
A Strict Complete Response (CRs) is defined by the following criteria:
The reaction is complete.
There are no myeloma cells in the bone marrow.
Complete answer
A complete response (CR) is defined by one of the following criteria:
During immunofixation, a specialized type of electrophoresis that identifies the type of M protein or immunoglobulin light chain, M protein is not detected in blood or urine;
an extramedullary plasmacytoma has disappeared;
plasma cells make up 5% or less of the cells in the bone marrow.
Very good partial response
A very good partial response (TBRP) is defined by one of the following criteria:
In immunofixation, M protein is detected in blood or urine, but M protein is not detected by standard electrophoresis.
The blood level of M protein has dropped by at least 90% and the urine level of M protein is less than 100 mg (urine collection over 24 hours).
Partial response
A partial response (PR) is defined as follows:
- The blood level of M protein has dropped by at least 50%, and the urine level of M protein has dropped by more than 90% or is less than 200 mg (urine collection over a 24 hour period).
- If M protein cannot be measured in blood and urine, RP is defined as a minimum 50% decrease between the levels of the free light chains (Bence-Jones proteins) involved and not involved.
- If M protein and free light chains cannot be measured, PR is defined as a minimum 50% decrease in plasma cells
- in the bone marrow (if the baseline percentage of plasma cells in the bone marrow was at least 30 %).
- If an extramedullary plasmacytoma was detected at the time of diagnosis, it has shrunk by more than 50%.
Progressive disease
Progressive disease (PD) is defined by one or more of the following criteria:
The level of M protein in the blood or urine, or both, has increased by at least 25%, or the percentage of plasma cells in the bone marrow has increased by at least 25% (plasma cells are at least 10% % of all cells in the bone marrow), or both.
You have new abnormal bone areas or plasmacytomas.
You have hypercalcemia, which is a high level of calcium in the blood, linked to multiple myeloma.
Stable disease
The disease is said to be stable (MS) when it does not meet the criteria of the categories described above.
Supportive care for multiple myeloma
Supportive care empowers people to overcome the physical, practical, emotional and spiritual barriers created by multiple myeloma. It is an important component of the care of people with this disease. There are many programs and services that help meet the needs and improve the quality of life for these people and their loved ones, especially after treatment is over.
Recovering from multiple myeloma and adjusting to life after treatment is different for everyone, depending on the extent of the disease, the type of treatment given and many other factors. The end of cancer treatment can lead to mixed emotions. Even if the treatment is finished, there may be other issues that need to be addressed, such as coping with long-term side effects. A person who has been treated for multiple myeloma may be concerned about the following.
Fatigue and anemia
Fatigue is a symptom of a low number of red blood cells (anemia). There may be a low number of red blood cells in the bone marrow when there is a high number of plasma cells (myeloma cells). Fatigue can also be a symptom of treatment for multiple myeloma or of other problems, including malnutrition, sleep disturbances, stress, anxiety and depression.
Once the cause of fatigue is known, your healthcare team can suggest ways to deal with it, including the following:
- nutritional supplements if you are malnourished;
- iron pills or blood transfusion for anemia;
- medicines that help the body make more red blood cells (erythrocyte growth factors);
- antidepressants for depression;
- sleeping pills to help improve your sleep.
Infection
There may be a low number of white blood cells and a lower production of antibodies when multiple myeloma or its treatments affect the bone marrow. White blood cells as well as antibodies help fight infections. A low number of white blood cells or antibodies can lead to infection.
Preventing infections is important in people with multiple myeloma. Practicing good hygiene, protecting your skin, and maintaining good overall health are some of the ways you can help prevent infections. Your healthcare team may give you medicine to prevent infections or to increase your white blood cell count if your number is low. You may be given the following:
antibiotics, antivirals and antifungals – to treat infections;
colony stimulating factors, such as filgrastim (Neupogen) or pegfilgrastim (Neulasta) – to increase the number of white blood cells.
Your doctor may also suggest that you get the pneumococcal pneumonia and influenza (flu) vaccine to help reduce your risk of getting an infection.
Bone pain and fractures
Bone pain is a common symptom in people with multiple myeloma. Bone pain can be the result of the buildup of myeloma cells in the bones. It can also happen if a bone breaks down or is fractured (broken). Treatments that aim to prevent bone pain and fractures may include the following:
- radiotherapy;
- bisphosphonates;
- painkillers.
You may be given pain relievers such as acetaminophen (Tylenol), dihydrocodeine, morphine (MS Contin), or fentanyl (Duragesic). However, nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Motrin, Advil) or naproxen (Naprosyn, Aleve) are usually not given to people with multiple myeloma since these drugs may increase the risk. kidney damage.
Nerve blockage
This procedure blocks pain by injecting local anesthetic (numbing agent) and other medicines into or around a nerve or into the space around the spinal cord.
Vertebroplasty
Bone cement is injected into the fractured vertebra to stabilize it so that it does not move.
Kyphoplasty
When part of a vertebrae collapses, a balloon is inserted into the collapsed area to lift it. Bone cement can then be injected into the area that was sagging to stabilize the vertebra.
Neuralgic pain and peripheral neuropathy
Fractured bones can cause nerves to compress, which can cause nerve damage and pain. Treatments for nerve pain may include administering pain relievers, such as gabapentin (Neurontin), amitriptyline (Elavil) or pregabalin (Lyrica).
Vertebroplasty and kyphoplasty can also help reduce the pressure on nerves that are compressed due to a fractured bone, thus reducing neuralgia pain.
Some medicines used to treat multiple myeloma, such as thalidomide (Thalomid) and bortezomib (Velcade), can cause peripheral neuropathy. Peripheral neuropathy causes pain, a burning sensation, numbness, or tingling in the hands, arms, feet, or legs. Treatments for peripheral neuropathy include the following:
- administration of painkillers, such as gabapentin (Neurontin), amitriptyline (Elavil) or pregabalin (Lyrica);
- reducing the dose of drugs given to treat multiple myeloma;
- changing the frequency with which drugs to treat multiple myeloma are given;
acupuncture.
Although there hasn’t been a lot of research, there is some evidence that acupuncture can help relieve peripheral neuropathy.
If the peripheral neuropathy is severe, your doctor may need to stop treatment for a while.
Hypercalcemia
Multiple myeloma can cause bone breakdown. When bones break down, calcium enters the bloodstream. This can lead to an increase in the level of calcium in the blood, a condition called hypercalcemia. You may feel constipated, need to urinate often, or feel weak or confused. Treatment for hypercalcemia may include the following:
- taking bisphosphonates;
- consuming a large amount of fluids;
- administration of fluids into a vein (intravenous).
Kidney problems
Some people with multiple myeloma have kidney problems because they have high calcium levels in their blood (hypercalcemia) or because M proteins have built up in a kidney. It may cause kidney damage. You will have regular tests to check how well your kidneys are working. If you have kidney problems, treatment may include the following:
- Chemotherapy – which kills the myeloma cells responsible for making M proteins and breaking down bones
- Consumption of a large amount of fluids
- Taking bisphosphonates
- Plasmapheresis – a treatment used to remove plasma from the blood if it contains a lot of M protein and becomes too thick (a condition called hyperviscosity)
- Dialysis – to purify the blood of wastes if the kidneys are severely damaged and no longer functioning
- Kidney transplant – may be needed in rare cases if the kidneys are severely damaged and are no longer functioning
Hyperviscosity
Hyperviscosity is when the blood has grown too thick (viscous). This condition can occur when there is a large amount of M protein in the blood. Hyperviscosity can make you feel dizzy, weak and tired and can cause headaches. The treatment for hyperviscosity is called plasmapheresis, which removes the plasma that contains M proteins from the blood.
Plasmapheresis lowers protein levels; but without further treatment, the protein level will rise again. After plasmapheresis, you may be given chemotherapy or other drug therapy to reduce the number of myeloma cells that make M proteins.
Osteonecrosis of the jaw
Bisphosphonates can cause the death of bone tissue in the jaw, a condition called osteonecrosis of the jaw. This is a rare side effect of bisphosphonates and doctors do not know why it happens. This effect is more common in people who have had dental surgery such as tooth extraction or periodontal surgery (implantation, for example). Symptoms of osteonecrosis of the jaw include pain, swelling, tooth mobility (loosening), numbness of the jaw, poor healing and infection. Treatments for osteonecrosis of the jaw may include the following:
- Antibiotics
- Mouthwash
- Prosthesis in the mouth
- Surgery to remove the affected bone or tissue
- Surgery can make osteonecrosis of the jaw even worse, so it is only done when clearly needed.
People should have a complete dental check-up before taking bisphosphonates. It is very important that people with multiple myeloma who take bisphosphonates have a regular dental check-up. Any dental surgery should also be performed before taking bisphosphonates.
Emotional health
Emotions can be overwhelming during and after treatment. Many people with multiple myeloma feel anxious or depressed.
During treatment, the goal is to get through this step. Treatment takes a long time and it can be difficult to stay positive. You may have concerns about money, work, and your relationships with others.
After treatment, you may think of other things and experience unexpected emotions, including the following:
- worry about the recurrence of multiple myeloma;
- effects of multiple myeloma on your family, friends and career;
- questioning about your self-esteem and your identity;
- worry about changes in your appearance;
- adaptation to changes in your lifestyle;
- anxiety about less contact with the healthcare team.
People cope with multiple myeloma in different ways. You may find it helpful to:
- practice appropriate physical activities;
- have a good diet;
- strike a good balance between activity and rest;
- speak openly and candidly about your fears and concerns.
Treatment for emotional disorders may include counseling and medication.
Lifestyle change
Making certain lifestyle changes and developing a wellness plan may help you cope better with multiple myeloma. Lifestyle changes can help you stay healthy and feel better. You might find it helpful to:
- stop smoking;
- eat better;
- limit your alcohol consumption;
- to exercise.
However, some types of high impact exercise, such as jogging or contact sports, can lead to bone damage or fractures in people with multiple myeloma. Ask your doctor or physiotherapist what types of exercise are best for you.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Cancer Center, Web MD, American Cancer Society, European Society for Medical Oncology (ESMO), Cancer Council Australia, National Cancer Institute (NIH), International Agency for Research on Cancer, National Cancer Centre Singapore
Photo explanation: Illustration of the most common bone lesions in the vertebrae in patients with multiple myeloma.
Photo credit: Blausen Medical Communications, Inc. / Wikimedia Commons