Understanding Syphilis: Causes, Symptoms, and Treatment
Syphilis is a sexually transmitted infection (STI) caused by bacteria called Treponema pallidum. It starts with the appearance of a painless ulceration in the penis, vagina or anus. If left untreated, syphilis can cause serious health problems, affecting the heart and brain.
Important information: this article discusses: biology, health and anatomy of the human body. If you feel uncomfortable, please leave this page right now. Thank You!
Signs and Symptoms
It has 3 stages as well as a latency period. The primary, secondary and early latent stages of syphilis are considered infectious. Each stage has different symptoms.
5 Main Stages of Syphilis
It has five main stages that show different symptoms and risks, as follows:
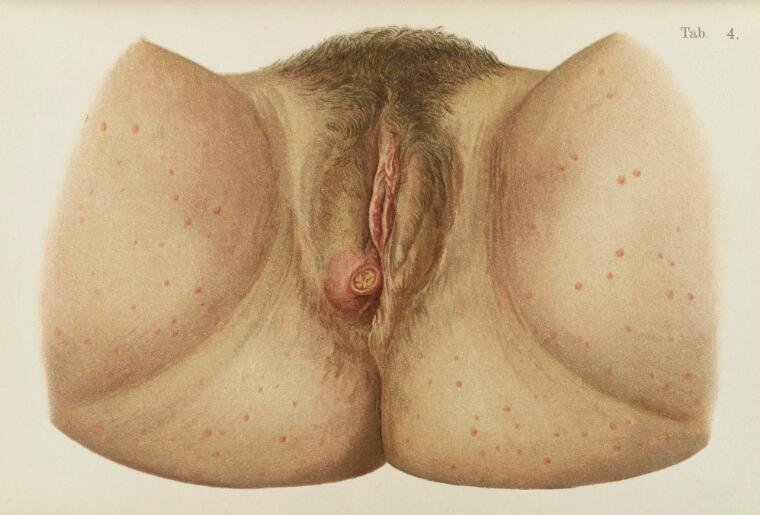
1. Primary stage (3 days – 3 months after exposure)
Symptoms first appear 3 to 90 days after infection, but usually 3 weeks.
- At first, the infection looks like a red pimple;
- The bacteria then multiply and eventually create a painless ulcer (s) at the site of infection, usually in the genital, anal or throat area. This ulcer is called a syphilitic chancre. It may be visible on the penis, but easily hidden in the vagina or anus, especially as it is painless. Most people who are infected develop only one chancre, but some develop more than one;
- The sore will eventually resolve on its own within a month or two. If it has not been treated, however, this does not mean that the infection is cured.

Primary stage syphilis sore (chancre) on the surface of a tongue. Centers for Disease Control and Prevention (CDC), Public domain, via Wikimedia Commons

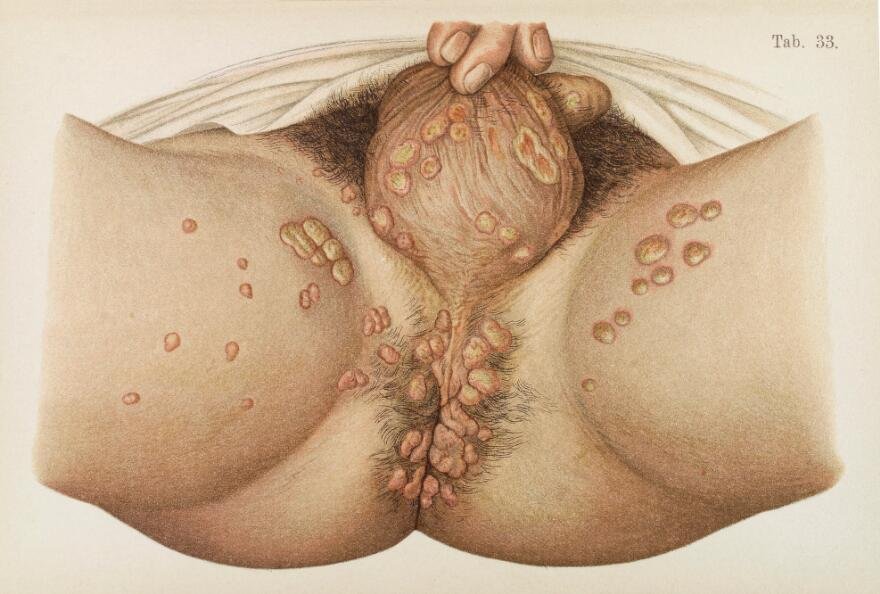
2. Secondary stage (6 weeks to 6 months after exposure)
When untreated, syphilis progresses. 2 to 10 weeks after the onset of ulcers, the following symptoms occur:
- Fever, fatigue, headache and muscle pain;
- Hair loss (alopecia);
- Redness and rash on the mucous membranes and skin, including on the palms of the hands and soles of the feet;
- Inflammation of the lymph nodes;
- Inflammation of the uvea (uveitis), the vasculature of the eye, or the retina (retinitis).
These symptoms may go away on their own, but it does not mean that the infection is cured. They can also appear and reappear intermittently, for months or even years.

Dorsal syphilitic lesions in secondary syphilis. See page for author, Public domain, via Wikimedia Commons

3. Latency period (without syphilis symptoms)
After about 2 years, syphilis goes into a latent state, when no symptoms appear. However, the infection can still develop. This period can last from 1 year to 30 years.
4. Tertiary stage or third stage (2 to 30 years or older)
If left untreated, 15-30% of people infected with syphilis will experience very serious symptoms which in some cases can even lead to death:
- Cardiovascular syphilis (inflammation of the aorta, aneurysm or aortic stenosis, etc.);
- Neurological syphilis (stroke, meningitis, deafness, visual disturbances, headache, dizziness, change in personality, dementia, etc.).

5. Congenital syphilis
Treponema is transmitted from the infected mother through the placenta and will lead to miscarriages, neonatal deaths. Most affected newborns will not have any symptoms at birth, but they will appear within 3 to 4 months;
Gum: destruction of tissue in any organ.

The face of a newborn infant displaying snuffles indicative of congenital syphilis. CDC/ Dr. Norman Cole, Public domain, via Wikimedia Commons
People at risk
- People who have unprotected sex;
- People who have more than one sexual partner;
- People with HIV or other STIs;
- People who inject drugs and their partners.
Syphilis and pregnancy
Screening for congenital syphilis should be done in the first trimester of pregnancy. If this could not be done or if the patient is at risk, it is recommended to do a third trimester screening.
- Can occur with untreated maternal / congenital syphilis:
- Low birth weight,
- Sequelae of the newborn (deafness, visual disturbances, malformations, etc.),
- Premature delivery,
- Fetal death.
Read also: Pregnancy superstitions and beliefs: should we believe them?

Severe facial disfigurement caused by congenital syphilis, 1880. G. H. Fox, Public domain, via Wikimedia Commons
Prevention of Syphilis
Why prevent?
Prevention aims to reduce the incidence of syphilis by preventing the transmission of the bacteria.
Basic preventive measures
Using condoms correctly helps prevent the transmission of syphilis during anal or vaginal sex. Condoms or dental dams can also be used as a means of protection during oral sex.
Screening measures
Systematic screening for syphilis at the 1st pregnancy visit:
Given the resurgence of syphilis in Canada, but also in the United States, Asia, Africa and Europe, systematic screening is essential for all pregnant women.
Screening for unprotected sex
Getting tested helps prevent the infection from being passed on to new partners. If you test positive, tell anyone you have had sex with who may have been exposed. This person will need to be tested and treated, if necessary.
Syphilis can be detected with a blood test.
Regular testing for syphilis is advised in people who have unprotected sex. It is compulsory for pregnant women during the first prenatal examination.
SCREENING FOR ACQUIRED SYPHILIS
Because syphilis is highly contagious, testing and treating patients with syphilis helps prevent new cases from occurring in sexual partners and this can be transmitted from person to person by direct contact with a syphilitic sore.
Screening by serological test (blood test) is recommended and may be offered annually to certain groups of the population having unprotected sex, including fellation:
- sharing sex toys;
- sex workers;
- people who associate with sex workers;
- people who have relationships with more than one partner over the year.
Screening is also important for:
- people at risk, having had unprotected sex or having been in contact with a syphilitic subject;
- when diagnosed or if there is a history of gonorrhea type STIs, lymphogranulomatosis venereal disease and HIV infection;
- among migrants from endemic countries: Africa, Asia, Eastern Europe, South America;
- during incarceration (imprisonment);
- after rape.
Screening is mandatory in the event of blood donation.
Male Condom | Advantages and Disadvantages ? | How to use it, accidents
SCREENING FOR SYPHILIS IN PREGNANT WOMEN
Screening is mandatory for pregnant women, ideally during the first 3 months of pregnancy. This examination is carried out during the first prenatal examination.
Screening is repeated during the 3rd trimester, ideally before the 28th week of pregnancy, in women at risk. That is, pregnant women:
- having unprotected sex with a new partner after the first screening;
- whose the partner is in this situation.
Female Condom | Advantages and Disadvantages ? | How to use it, accidents
Medical treatments
Syphilis is treated with antibiotics, usually penicillin, by intramuscular injection. If you are allergic to penicillin, other antibiotics are available.
If the infection has lasted for less than 1 year, a single dose may be sufficient. Further blood tests will be done after treatment to check if the antibiotics have been working. Immunosuppressed people, especially those with HIV, may need longer treatment.
The treatment modalities (in particular the dosage) vary according to the primary, secondary or tertiary nature of the syphilis.
1. Primary syphilis:
1 single intramuscular injection of benzathine-penicillin. In case of allergy, macrolides or cyclins for 15 days orally.
2. Secondary syphilis:
3 intramuscular injections one week apart of benzathine-penicillin or one injection of depot penicillin. In case of allergy, macrolides or cyclins for 15 days orally.
4. Tertiary syphilis (neurological impairment):
3 injections of benzathine-penicillin one week apart, or penicillin G intravenously for 15 days.
4. Treatment of tertiary syphilis or late latent syphilis
In the case of non-neurological tertiary type or late latent type, the treatment is longer and is based on an intramuscular injection of benzathine penicillin G “retard” per week, for 3 weeks.
The treatment of a pregnant woman at this syphilitic stage is the same as for any other infected person.
In case of neurosyphilis, hospitalization is necessary. For 14 days, the patient receives an intravenous infusion of 20 million units of penicillin G per day. The effectiveness of this treatment is 100%. However, there is no alternative treatment for penicillin allergy. However, there is still the possibility of inducing tolerance to penicillin by administering small doses of penicillin a few days before treatment.
One of the side effects of the treatment is the Herxheimer reaction is the sudden worsening of symptoms 6 to 12 hours after the first dose of the antibiotic (fever, malaise, muscle pain). To avoid this reaction, corticosteroids are given 48 hours before the start of antibiotic therapy.
Sources: PinterPandai, NHS UK, National Institute of Allergy and Infectious Diseases (NIAID)
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.



