Mycoplasmas Infections
Mycoplasmas are small widespread bacteria that cause respiratory or urogenital (relating to the organs that remove liquid waste from your body and to your sex organs) infections in humans. More than a hundred Mycoplasma species are known.
This is the case with Mycoplasma genitalium which causes sexually transmitted infections (STIs) or Mycoplasma pneumoniae which causes respiratory infections. These two species are considered from the outset to be pathogenic for humans.
Other species are considered commensal, that is to say, colonizing the body without necessarily presenting an infectious character. It is estimated that 50% of women are colonized by mycoplasmas.
Mycoplasmas are small bacteria responsible for infections of the male genital tract, gynecological or extra-genital infections, reproductive disorders, neonatal or respiratory infections.
Read also: Infectious Diseases and Contagious (viruses, bacteria, parasites, fungi, protozoa)
Mycoplasmas: What are they?
Mycoplasmas are small bacteria widely distributed in nature and belonging to the Mollicutes family. Respiratory mycoplasmas and genital mycoplasmas are distinguished in humans.
Mycoplasma pneumoniae is a respiratory mycoplasma. It is most often responsible for tracheobronchitis. More exceptionally, it can infect the urogenital tract. Other respiratory mycoplasmas exist but are not pathogenic to humans.
In the urogenital tract, certain species are present in the commensal state: this is called colonization. This is the case with Mycoplasma hominis and Ureaplasma urealyticum which can potentially become pathogenic in some cases. In the case of Mycoplasma genitalium, its presence is considered to be pathogenic from the outset.
Mode of transmission of Mycoplasmas
Mycoplasma pneumoniae
Mycoplasma pneumoniae does not belong to the commensal flora of the respiratory tract. Transmission occurs through contact with infected patients through droplets excreted by them during sneezing, etc.
Infections appear as an epidemic every 3 to 5 years and preferably in the fall.
Urogenital mycoplasmas
While Mycoplasma genitalium is considered responsible for sexually transmitted infections (STIs), Mycoplasma hominis and Ureaplasma urealyticum are not the cause of the genital tract.
In France, it is estimated that 50% of women are carriers of Ureaplasma urealyticum and 10% for Mycoplasma hominis. This carrying has no impact on their health and is usually asymptomatic.
Transmission can be from mother to newborn during childbirth.
Symptoms of Mycoplasma infections
Symptoms depend on the species infecting the patient and the location: respiratory or urogenital.
Mycoplasma pneumoniae
Mycoplasma pneumoniae is responsible for respiratory infection.
Most often, it is tracheobronchitis (chest cold). Children and young adults are the most affected.
The most characteristic form is atypical pneumonia. It most often begins with a dry sore, ENT signs and fever. More rarely, it is accompanied by an extra-respiratory sign (cutaneous, articular, neurological and / or pericardial).
It is considered that 15 to 20% of community infections are due to Mycoplasma pneumoniae.
Urogenital mycoplasmas
If Mycoplasma genitalium is considered pathogenic, it is different for Mycoplasma hominis and Ureaplasma urealyticum which are commensals of the genital tract. To be considered pathogenic, these two species must be isolated at a high concentration (minimum 104 CCU / ml).
Mycoplasma hominis
In humans, Mycoplasma hominis does not appear to have a pathogenic role.
In women, the attacks concern the cervix (cervicitis), the tubes (salpingitis), the endometrium (endometritis) and more exceptionally the pelvic region.
In addition, this species is implicated in cases of bacterial vaginosis even if they are not the only cause.
Ureaplasma urealyticum
In humans, Ureaplasma urealyticum is responsible for non-gonococcal urethritis, more exceptionally epididymitis or prostatitis.
In women, endometrial damage (endometriosis) is possible.
Mycoplasma genitalium
Mycoplasma genitalium is initially considered to be pathogenic. The symptoms are very similar to those caused by Chlamydiae trachomatis infections.
In men, the infection is responsible for urethritis or more simply for urination burns. More rarely, it can be the cause of prostatitis or epididymitis.
In women, the infection is responsible for cervicitis, endometritis and salpingitis. It is also implicated in some cases of bacterial vaginosis.
Extrogenital damage is possible for these mycoplasmas usually responsible for urogenital damage.
Urogenital mycoplasmas and pregnancy
Vaginal colonization is common during the pregnancy. It can affect up to 50% of pregnant women for Mycoplasma hominis, and up to 80% for Ureaplasma urealyticum.
If mycoplasmas can be considered responsible for premature delivery, rupture of membranes or postpartum endometriosis, to date, current knowledge does not allow us to confirm this. Other bacteria associated with mycoplasmas could be responsible.
Laboratory diagnosis of Mycoplasma infections
Culture cells in the laboratory
The culture is carried out from biological samples (first urine sample, vaginal sample, urethral sample, etc.) and makes it possible to isolate the Mycoplasma hominis and Ureaplasma urealyticum strains.
As mentioned above, their presence does not necessarily indicate infection. Mycoplasmas may be present in the commensal state, but a concentration greater than 104 CCU / ml is indicative of infection.
Culture for Mycoplasma genitalium and Mycoplasma pneumoniae is not performed routinely because it is longer and more difficult.
Gene amplification by PCR (Polymerase Chain Reaction)
The PCR technique allows the diagnosis of Mycoplasma genitalium infection directly from biological media (first urine stream, urethral sample, etc.).
In practice, PCR is rarely carried out because it is expensive and not reimbursed by health insurance.
The PCR technique is also applicable to other genital mycoplasmas and to Mycoplasma pneumoniae but difficult to implement routinely and therefore little or not practiced.
Serology (diagnostic identification of antibodies in the serum)
Serology is performed from blood taken from the patient. It consists in demonstrating the presence of specific antibodies vis-à-vis the mycoplasmas sought.
It is usually recommended to perform two serologies, spaced 2 to 3 weeks apart, in order to assess the evolution of the antibody levels. Evolution which makes it possible to confirm or not the diagnosis of active infection.
While serology is the most widely used to diagnose Mycoplasma pneumoniae infection, it is, on the other hand, rarely performed for genital mycoplasmas.
Treatment of Mycoplasma infections
Treatment is based on oral administration of an antibiotic. There is no vaccine to prevent infection with mycoplasmas.
In the event of an uncomplicated infection, two antibiotic protocols can be offered as first-line treatment and without waiting for the resistance profile:
- azithromycin for 5 days (500 mg then 4 x 250 mg);
- doxycycline for 7 days (100 mg twice daily) followed by 3 days of azithromycin (1 g then 2 x 500 mg) (grade 1D).
In the second protocol, treatment with azithromycin can be postponed for a few days while awaiting the results of the antibiogram.
If the mycoplasma is resistant to macrolides, or if azithromycin has failed (without an antibiogram supporting resistance), the recommended treatment is moxifloxacin for 10 days (400 mg / day, grade 1D).
In the event of complications or rectal infection, the moxifloxacin-based protocol should be extended for a total of 14 days (grade 1B).
What to do in case of failure?
If treatment fails, experts insist on not repeating treatment with azithromycin. Therefore, the often prescribed single-dose treatment (see for example on Antibioclic) should no longer be prescribed, in favor of the 5-day treatment in case of failure.
Moxifloxacin remains effective in Europe but presents many resistance in the Pacific area due to more common use.
Alternative protocols are also proposed based on pristinamycin and minocyclineNational Center for Biotechnology Information (NCBI), .
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Official New York State Portal, Web MD, StatPearls Publishing LLC / National Center for Biotechnology Information (NCBI), BMJ Publishing Group
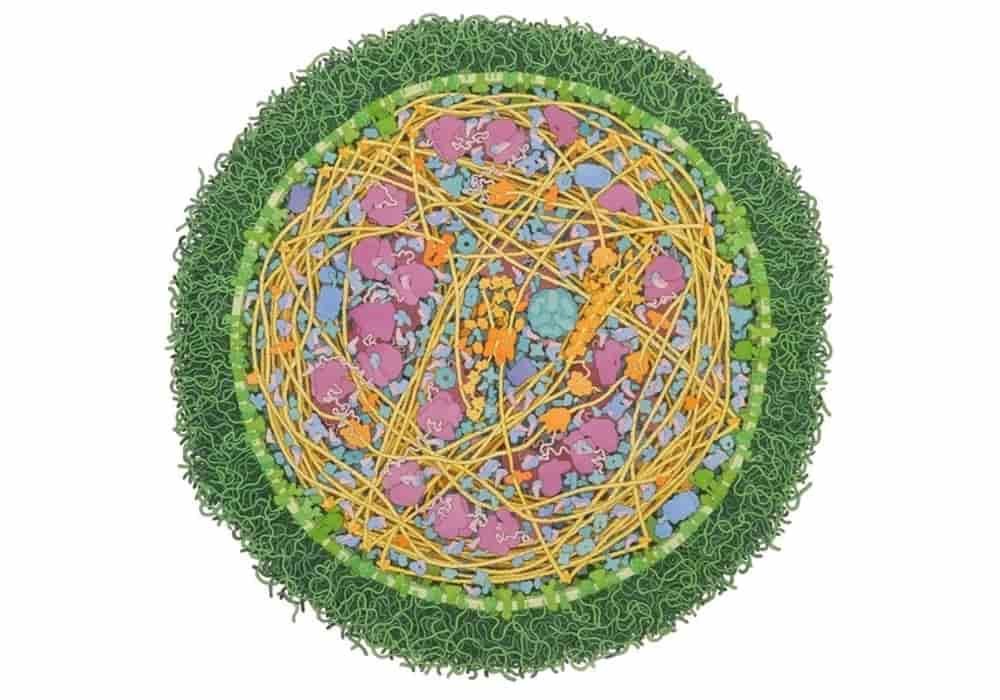
Photo credit: National Science Foundation / David Goodsell / Wikimedia Commons (CC BY 4.0)
Acknowledgement: Illustration by David S. Goodsell, The Scripps Research Institute. doi: 10.2210/rcsb_pdb/goodsell-gallery-011
Photo explanation: in this illustration shows an entire mycoplasma cell, created in collaboration with Field Test Independent Film Corps. The cell shown here is about 300 nanometers in diameter, which is at the small end of the range of observed sizes.