Lymphoma
Lymph node cancer, also known as lymphoma, is a type of cancer that originates in the lymphatic system. Lymphoma is group of blood cancers. Lymphoma is cancer of the lymphatic system at the expense of lymphocytes.
The lymphatic system includes the bone marrow, spleen, thymus gland, lymph nodes and lymphatic vessels; it defends the body against microbes, parasites, toxins, foreign bodies, etc.
The difference between Hodgkin lymphoma and Non Hodgkin lymphoma (NHL) is the presence of Reed-Sternberg cells. A Reed-Sternberg cell is a cell derived from a B lymphocyte that is only present in Hodgkin lymphoma.
Lymphomas are among the cancers that are treated with modern treatments such as chemotherapy, radiotherapy and immunotherapy. The response to treatments for different lymphomas depends on the type and stage of the lymphoma, as well as a number of other factors.
Difference between Hodgkin lymphoma and non-Hodgkin lymphoma
What is a cancer cell?
Our cells divide to ensure the growth and renewal of tissues in our body. This process is orchestrated, in each cell, by a set of genes. A cancer cell is a cell that has suffered a genetic accident. The process of division can then become uncontrollable: the cells multiply in an anarchic way, and the resulting cells will in turn multiply in excess. In some cases, these cells become immortal and this accumulation of abnormal cells creates the malignant tumor.
Hodgkin lymphomas
Hodgkin lymphoma (or Hodgkin lymphoma) is a special form of lymphoma. It was first described in 1832 by Thomas Hodgkin, an English physician who found under a microscope the presence of an abnormally large cell (Sternberg cell) characteristic of this type of cancer.
Non-Hodgkin lymphomas
Besides Hodgkin lymphomas, there are many other lymphomas, linked to the proliferation of other types of cells. They are grouped under the name of “non-Hodgkin lymphoma”. This heterogeneous set includes about 30 different lymphomas. Each has its own characteristics. To facilitate their management, non-Hodgkin lymphomas are classified into different groups.
We distinguish lymphomas which derive from:
- very immature cells, found in the bone marrow,
- mature cells, found in the blood or lymph nodes.
We also distinguish lymphomas from:
- B lymphocytes, which produce our antibodies,
- T lymphocytes, which do not produce antibodies but also play an important role in immunity.
What is Hodgkin lymphoma?
Hodgkin lymphoma (HL) is a cancer that starts in lymphocytes. Lymphocytes are a type of white blood cell found mostly in the lymphatic system.
The lymphatic system is an important part of the immune system, which helps the body fight infections and disease. The lymphatic system is made up of lymph, lymphatic vessels, lymph nodes and lymphatic organs found throughout the body. LH can appear anywhere in the lymphatic system. It usually starts in a group of lymph nodes in one part of the body, most often the chest, neck or armpits.
There are 2 types of lymphocytes, namely B lymphocytes, or B cells, and T lymphocytes, or T cells. LH usually starts in abnormal B lymphocytes, which are called Hodgkin cells and Reed-Sternberg, or HRS cells.
Hodgkin lymphoma is divided into 2 main forms which are based on the presence of HRS cells. Classical LH contains many HRS cells, but lymphocyte-predominantly nodular LH does not contain HRS cells.
LH can cause generalized symptoms, which means it affects the whole body. These are called B symptoms, or systemic symptoms. These symptoms are unexplained fever, night sweats, and weight loss. The presence of any of the B symptoms can help predict the outcome of the disease. If you don’t have B symptoms, the outcome is better.
Classic LH
Classical LH is the most common type of LH (it is also sometimes just called LH). About 95% of all LH are classic. Classical LH contains HRS cells. Classic LH is divided into 4 subtypes.
Scleronodular LH is the most common type of LH (about 60-70% of all cases). It is most often seen in adolescents and young adults between the ages of 15 and 34. Scleronodular LH usually starts in lymph nodes in the deep tissue of the central part of the chest (mediastinum) or neck.
Mixed cellularity HL is the second most common type of LH (about 25% of all cases). It is most often seen in children and adults between the ages of 55 and 74. It affects men more than women. This is the type of LH that appears most frequently in people with HIV. Mixed cellularity HL usually occurs in the upper half of the body and often in the lymph nodes in the abdomen and spleen. It usually causes B symptoms.
LH rich in lymphocytes accounts for about 4% of all cases. It usually starts in the lymph nodes in the neck, armpit and above the collarbone. It is rare that more than a few nodes are affected. It usually does not cause B symptoms.
Lymphocyte-depleted LH is the least common type of LH (only about 1% of cases). It can be seen in people with HIV. Lymphocyte-depleted LH usually affects only the lymph nodes in the chest, abdomen, spleen, liver, and bone marrow. Most people with the disease have B symptoms.
Lymphocyte-predominantly nodular LH
Lymphocyte-predominantly nodular LH accounts for about 5% of all cases of LH. This type of LH does not contain HRS cells. But it contains abnormal cells called LP cells, or “popcorn” cells because they look like popcorn when viewed under a microscope.
Lymphocyte-predominantly nodular HL is more common in adults between the ages of 30 and 50. It affects men more. It usually starts in the lymph nodes in the neck, armpit or groin. Usually it develops slowly (indolent) and is at an early stage when diagnosed. Most people with the condition have no symptoms other than swollen lymph nodes. B symptoms are rare.
The other main form of cancer of the lymphatic system is non-Hodgkin lymphoma (NHL). Abnormal Hodgkin lymphoma B cells look and behave differently from non-Hodgkin lymphoma cells. Hodgkin lymphoma and non-Hodgkin lymphoma are treated differently.
It’s important to talk to your healthcare provider if you are experiencing any symptoms of lymph node cancer or have any concerns about your risk of developing the disease.
Risk factors for Hodgkin lymphoma
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors, but Hodgkin lymphoma (HL) can develop in people who do not have any of the risk factors described below.
HL affects men slightly more often than women. It appears mostly in young adults (mid-teens to their 30s inclusive) and in people 55 years of age and older.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
Risk factors:
Epstein-Barr virus infection
Family history
HIV infection
There is convincing evidence that the following factors increase your risk for LH.
Epstein-Barr virus infection
Long-term infection with Epstein-Barr virus (EBV) is a risk factor for LH. VEB is a type of herpes virus that causes infectious mononucleosis (also called mono, or kissing disease). A large number of people are infected with EBV, but only some of them develop a long-term infection.
Family history
First-degree relatives of someone with HL, especially same-sex siblings, are at increased risk of developing the disease. It is not clear whether this higher risk is attributable only to genetics or if it is due to a combination of genetics and exposure to similar environmental factors.
HIV infection
The human immunodeficiency virus (HIV) is the virus that causes AIDS. HIV weakens the immune system and can make a person vulnerable to certain types of cancer, including Hodgkin’s LH. The risk of LH is 10 times higher in people with HIV than in people without.
Possible risk factors
The following factors have been linked to some extent with HL, but there is insufficient evidence to suggest that they are risk factors. More research is needed to clarify the role of these factors in the development of HL:
- certain genetic factors
- infectious mononucleosis
- autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, ulcerative colitis, sarcoidosis, and immune thrombocytopenic purpura
- immune deficiency (poor functioning of the immune system)
- smoke tobacco
- socio-economic status and family types, for example higher social class, having fewer brothers, sisters and friends, low number of occupants in a house or low birth order
No link to Hodgkin lymphoma
Significant research shows no link between LH and radiation exposure.
Reduce the risk of Hodgkin lymphoma
You can reduce your risk for Hodgkin lymphoma (HL) by adopting the following behaviors.
Protect yourself against HIV and EBV infections
You can reduce your risk of getting HIV infection by avoiding activities that increase your risk of HIV, such as injecting drugs or having condomless sex with many partners.
To help reduce the risk of Epstein-Barr virus (EBV) infection, do not share drinks, food, utensils, or toothbrushes.
Live smoke-free
Smoking tobacco can increase your risk for LH. If you smoke, get help quitting.
Find out if your risk for Hodgkin lymphoma is high
Some people may be at higher than average risk for developing HL. Discuss your risk with your doctor. If it is above average, you may need to see your doctor more often to check for HL. Your doctor will tell you which tests to take and how often.
Symptoms of Hodgkin lymphoma
The signs or symptoms of Hodgkin lymphoma (HL) can vary depending on the location of the cancer in the body. Other medical conditions can cause the same symptoms as LH.
The most common symptom of HL is swelling of the lymph nodes in the neck, armpit, groin or chest. Swollen lymph nodes are usually painless, but the areas where the lymph nodes are affected sometimes become painful after drinking alcohol.
Here are other common symptoms of HL:
- fever
- night sweats
- weightloss
- itchy skin
- tired
- loss of appetite
- shortness of breath, cough, or wheezing
Symptoms B
Some symptoms of LH are generalized, which means they affect the whole body. These are called B symptoms, or systemic symptoms:
- fever with no apparent cause – your temperature may be high for several days or it may go from normal to below normal for days or weeks
- night sweats so bad that your sheets or clothes are wet and need to be changed
- unexplained weight loss of at least 10% of your body weight over a 6 month period
It’s important to talk to your healthcare provider if you are experiencing any symptoms of lymph node cancer or have any concerns about your risk of developing the disease.
Diagnosis of Hodgkin lymphoma
Diagnosis is the process of identifying the cause of a health problem. The diagnostic process for Hodgkin lymphoma (HL) usually begins with a visit to your family doctor. He will ask you about your symptoms and may do a physical exam. Based on this information, your doctor may refer you to a specialist or order tests to check for HL or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay to worry, but try to remember that other medical conditions can cause HL-like symptoms. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of HL.
The following tests are usually used to rule out or diagnose HL. Many tests that can diagnose cancer are also used to determine the stage, that is, how far the disease has spread. Your doctor may also give you other tests to check your general health and to help plan your treatment.
Health history and physical examination
Your health history consists of a checkup of your symptoms, your risks, and any medical events and conditions you may have had in the past. Your doctor will ask you questions about your history:
- Symptoms that suggest HL
- Epstein-Barr virus (EBV) infection
- HIV or AIDS
Your doctor may also ask you questions about your family history of LH.
The physical exam allows your doctor to look for any signs of LH. During the physical examination, your doctor may:
- Check if any lymph nodes are larger than normal (swollen).
- Feel your abdomen to see if the spleen or liver is larger than normal.
- Listen to your lungs to see if there is any trouble breathing.
Complete blood count
The complete blood count (CBC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. Doctors use it to rule out infection and to have baseline values against which to compare the results of future blood tests done during and after treatment.
Globular sedimentation rate
Doctors may order a blood test to find out the blood sedimentation rate (VSG). VSG measures the rate at which red blood cells, also called erythrocytes, fall to the bottom of a test tube. It is a general marker for inflammation. SVG may be higher than normal in some people with HL.
Blood biochemical analyzes
A blood chemistry test measures the level of chemicals in the blood. It makes it possible to assess the quality of functioning of certain organs and also to detect anomalies. To help determine the stage of LH, the following blood chemistry tests can be done.
Lacticodehydrogenase (LDH) helps assess how well the liver is working and shows the presence of cell damage. LDH may be higher than normal in the presence of LH if the cancer is very active and has damaged cells.
Alanine aminotransferase (ALT) and aspartate transaminase (AST) are used to assess how well the liver is working. A higher than normal ALT or AST level may mean that the LH has spread to the liver.
Alkaline phosphatase is used to assess how well the liver is working and to check the bones. A higher than normal level of this enzyme may mean that the LH has spread to the liver or bones.
Serum creatinine is used to assess how well the kidneys are working. A higher than normal creatinine level in the blood can mean that the LH has damaged the kidneys.
HIV test
An HIV test can be done if doctors believe the LH is linked to an infection with HIV (human immunodeficiency virus). The HIV test is a blood test that measures the level of anti-HIV antibodies in the blood. A high level of these antibodies means that a person is infected with HIV.
Hepatitis B or C test
Blood tests can be done to see if you have hepatitis B or hepatitis C as these may affect the way the treatments work. Some chemotherapy drugs could cause problems if you have these infections. If you have hepatitis B or hepatitis C, your healthcare team may change your treatment plan, in order to make it more secure.
Pulmonary radiography
In an x-ray, low-dose radiation is used to produce images of parts of the body on film. A chest x-ray can check if any lymph nodes in the chest are larger than normal. It is also used to determine if LH has spread to the lungs.
CT scan
A computed tomography (CT) scan uses special x-ray machines to produce 3-dimensional and cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the photos into detailed images.
A CT scan may be used to see if any lymph nodes are swollen or if there is a lump in the neck, chest, abdomen or pelvis. CT also allows doctors to see if a tumor is putting pressure on an organ or large blood vessel and if the disease is in the brain or near the spinal cord. A CT scan can also be done to see if the cancer has spread to organs, such as the lungs, liver or spleen.
CT is usually combined with PET (PET / CT) to get more information about the cancer.
Positron emission tomography (PET scan)
A positron emission tomography (PET) scan uses a type of radioactive sugar to detect changes in the metabolic activity of body tissues. A computer analyzes patterns of radioactivity distribution and produces 3-dimensional, color images of the region under investigation.
A PET can be used to find out if HL has spread from the location where it started to other areas of the body or to measure the effectiveness of treatment. It is normally combined with CT to have a more global picture and a 3D assessment of the disease.
Ultrasound
In an ultrasound, high-frequency sound waves are used to produce images of parts of the body. It can be used to examine the abdomen and organs that may be affected by LH, such as the kidneys, spleen or liver.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) uses powerful magnetic forces and radio waves to produce cross-sectional images of the body’s organs, tissues, bones, and blood vessels. A computer assembles the images into 3-dimensional snapshots.
An MRI may be used to check for swollen lymph nodes in the chest, abdomen or pelvis. It can also be used to find out if the cancer has spread to the brain or spinal cord. An MRI is usually not needed to assess LH, but an MRI can be done to see if the cancer has spread to bone or muscle tissue.
Biopsy
During a biopsy, the doctor removes tissues or cells from the body for analysis in the laboratory. The laboratory report will confirm the presence of cancer cells in the sample.
A swollen lymph node can be biopsied in the neck, armpit or groin. It is also possible to take a biopsy of a tumor in the chest or abdomen. The doctor may use computed tomography (CT) as a guide when biopsy of a lymph node in these areas.
The type of biopsy performed depends on where the doctor is to take the sample.
Surgical lymph node biopsy is usually done to collect samples from a lymph node. The surgeon may do an excisional biopsy, that is, remove an entire lymph node. In some cases, he may do an incisional biopsy, which is to remove part of the lymph node.
A core biopsy can be done for certain types of tumors, such as a large tumor in the chest or a bone tumor. The surgeon may use a CT scan to guide the needle to the tumor during a biopsy.
Immunophenotyping
Immunophenotyping is the study of proteins expressed by cells. It is based on a very specific antigen-antibody reaction to identify proteins in tissues or cells. Monoclonal antibodies labeled with a fluorescent substance or a specific enzyme that bind only to specific antigens (proteins) are used. The fluorescent marker and the marker enzyme allow doctors to observe lymphoma cells and determine the type of LH.
Immunohistochemistry is a method frequently used in immunophenotyping. We have recourse under a microscope to observe fluorescent markers. It also allows doctors to examine cells and their surroundings. Immunohistochemistry helps doctors determine the types of cells in a sample, including Hodgkin and Reed-Sternberg cells (HRS cells) and LP cells. Immunohistochemistry can eliminate LH. It can also lead to non-Hodgkin lymphoma or another disease.
Treatments for Hodgkin lymphoma
If you have Hodgkin lymphoma (HL), your healthcare team will create a treatment plan just for you. It will be based on your health and specific cancer information. When the healthcare team decides which treatments to offer for HL, they consider the following:
- the type of LH
- LH stadium
- areas of the body affected by HL
- the presence of B symptoms (specific symptoms that affect the whole body, such as fever)
- the presence of unfavorable (negative) risk factors, such as a tumor that is large (bulky)
- your age
- your overall health
- your risk of experiencing short-term or late side effects
Here is some general information about the treatments available for HL. Usually, LH is treated with chemotherapy, with or without radiation therapy. The treatment plan may be changed depending on your response to treatment.
Chemotherapy
Chemotherapy is the main treatment for HL. Chemotherapy uses cancer drugs to destroy cancer cells.
Radiotherapy
In radiation therapy, high-energy rays or particles are used to destroy cancer cells. It is sometimes given after chemotherapy to treat HL. It can be used on its own as the main treatment for early-onset LH if the lymphoma cells are found only in the area of the body where the cancer started (localized disease).
Stem cell transplant
A stem cell transplant can be done to treat refractory (unresponsive to treatment) or relapsing (comes back after treatment) HL.
In a stem cell transplant, a high dose of chemotherapy is given to destroy all the cells in the bone marrow. Healthy stem cells are then donated to replace those that have been destroyed in the bone marrow.
Targeted treatment
Targeted drugs and standard chemotherapy can be given to treat certain types of HL or LH that relapses or no longer responds to other treatments. Targeted therapy uses drugs to target specific molecules, such as proteins, present on the surface or inside of cancer cells in order to stop the growth and spread of cancer while limiting cell damage. normal.
Immunotherapy
Immunotherapy is a type of targeted therapy that helps strengthen or restore the ability of the immune system to find and destroy cancer cells. It can be combined with standard chemotherapy to treat HL that relapses or does not respond to other treatments.
If you cannot or do not want to be treated for cancer
You may want to consider care that aims to make you feel better without treating the cancer itself, perhaps because cancer treatments no longer work, or they are no longer likely to improve your condition, or cause them to work. secondary are difficult to tolerate. There may be other reasons why you cannot or do not want to be treated for cancer.
Talk to members of your healthcare team. They can help you choose advanced cancer care and treatment.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits, especially during the first 5 years after treatment. These visits allow the healthcare team to monitor your progress and to know how you are recovering from treatment.
Clinical tests
Ask your doctor if there are any clinical trials underway in your country for people with HL. Clinical trials aim to find new methods of preventing, detecting and treating cancer.
Follow-up after treatment for Hodgkin lymphoma
Follow-up after treatment for Hodgkin lymphoma (HL) is an important part of caring for people with Hodgkin’s lymphoma. Cancer specialists (oncologists, radiation therapists) and your family doctor often share this responsibility. Your healthcare team will talk to you to decide which follow-up meets your needs.
Don’t wait until your next scheduled appointment to report any new symptoms and any symptoms that don’t go away. Tell your healthcare team if you have the following symptoms:
- new lump or swelling
- fever that persists
- night sweats
- weight loss that happens for no reason
- itching
- shortness of breath
- abdominal pain or discomfort
The risk of HL coming back (recurring) is highest during the first 3 years after treatment, so close monitoring should be done during this time.
Planning of follow-up visits
Follow-up visits for HL are usually scheduled as follows:
- every 2 to 4 months in the 1st and 2nd year after treatment
- every 3 to 6 months during the 3 to 5 years
- at least once a year after the first 5 years
Progress of follow-up visits
During a follow-up visit, your healthcare team will usually ask you questions about the side effects of treatment and how well you are coping. You may also be asked if you are experiencing any new symptoms and if your vaccines are up to date.
Your doctor may do a physical exam, including:
- check if you have a fever, are short of breath and your heart is beating fast
- feel your neck, armpits and groin for swollen lymph nodes;
- feel your abdomen to see if any organs are swollen.
Examinations are often ordered as part of the follow-up. We could ask these:
- complete blood count (CBC) to check for abnormal blood cell counts
- blood chemistry tests to assess how well certain organs are working
- thyroid stimulating hormone (TSH) test to check how well your thyroid is working (if you have had radiation therapy to your neck)
- imaging tests, such as a chest x-ray, computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET) or ultrasound, to check if the spleen, liver, or lymph nodes are swollen (you only need
- x-rays or imaging tests if you have new symptoms)
- regular breast cancer screening tests, such as a mammogram (if you have had radiation therapy to your chest, you should start having mammograms 10 years after the radiation therapy or at age 40, whichever comes before)
Your doctor may order a bone marrow puncture and biopsy if your blood test results are abnormal or if you experience new symptoms.
If your healthcare team finds out that the cancer has come back, they will talk to you to plan your treatment and care.
Supportive care for Hodgkin lymphoma
Supportive care empowers people to overcome the physical, practical, emotional and spiritual barriers of Hodgkin lymphoma (HL). It is an important component of the care of people with this disease. There are many programs and services that meet the needs and improve the quality of life of these people and their loved ones, especially after treatment is over.
Recovering from HL and adjusting to life after treatment is different for everyone, depending on the location of the cancer in the body, the stage of the cancer, the type of treatment, and many other factors. The end of cancer treatment can lead to mixed emotions. Even if treatment is finished, there may be other issues to work out, such as coping with long-term side effects. A person who has been treated for HL may be concerned about the following.
Self-esteem and body image
Self-esteem is how we feel about ourselves. Body image is how we perceive our own body. HL and its treatments can affect a person’s self-esteem and body image. This is often because cancer or treatments can cause changes in the body such as the following:
- scars
- hair loss
- skin changes
- changes in body weight
- lymphedema
Some of these changes may be temporary. Others can last a long time or be permanent.
Tired
You may feel very tired if your red blood cell count is low (anemia). The number of red blood cells may be low when the bone marrow is affected by LH or its treatments.
Fatigue can also be a symptom of other problems that people with HL are at risk of experiencing, such as malnutrition, trouble sleeping, anxiety or depression.
After determining the cause of the fatigue, your healthcare team may suggest ways to treat it, including the following:
- iron tablets if your iron levels are low
- blood transfusion for anemia
- nutritional supplements
- sleeping tablets
- antidepressants
Infections
You may get infections if your white blood cell count is low (neutropenia). The number of white blood cells may be low when LH or its treatments affect the bone marrow. Your healthcare team may prescribe medicine to prevent infections if your white blood cell count is low. You will also be given medicines to treat infections, such as antibiotics, antivirals and antifungals.
Sometimes the immune system of people with HL does not work properly. Treatments for LH, such as chemotherapy, radiation therapy, or removal of the spleen (splenectomy), can also affect the immune system. People who have had their spleen removed may need certain vaccines to help boost their immunity.
Preventing infections is important in people with HL. Practicing good hygiene, protecting your skin, and maintaining good overall health are some of the ways you can help prevent infections. It is also important to keep your vaccines up to date to help prevent certain infections.
Cavities
Radiation therapy given to the head or neck area may increase the risk of tooth decay following treatment since the radiation can affect the salivary glands so that they do not produce enough saliva. It depends on the dose of radiation and the number of salivary glands in the treatment area. If there is less saliva in the mouth, cavities and gum disease can develop. These problems can lead to toothaches, tooth decay, and swollen, painful gums.
You can help prevent tooth decay by doing the following:
- have a complete dental examination and a good cleaning
- fill your cavities (fillings) before treatment
- practice good daily oral hygiene and receive fluoride treatments during and after treatment
- have a regular check-up and cleanse and deal with any problems that appear after treatment for HL
Thyroid gland disorders
People who receive radiation therapy to their neck are more likely to have hypothyroidism in the future. Hypothyroidism refers to insufficient production of thyroid hormone
not by the thyroid gland, which interferes with the normal functioning of the body. It usually appears 3 to 4 years after radiation therapy, but it can also occur later.
The healthcare team will regularly check the function of your thyroid gland. Some people will need to take thyroid hormone replacement therapy to regulate their thyroid gland.
Fertility disorders
Some combinations of chemotherapy drugs and radiation therapy to the pelvis and surrounding areas may affect your fertility (ability to get pregnant or carry a pregnancy to term, or ability to make someone else pregnant).
Women who are naturally approaching menopause are the most likely to become infertile, as some LH treatments can cause early menopause. Younger women treated for HL may experience symptoms of menopause and become temporarily infertile. They are more likely than older women to become fertile again after treatment.
Some treatments for LH reduce or interrupt the production of sperm in the testes, which can cause temporary or permanent infertility in men.
Discuss your fertility with your healthcare team before starting treatment. There may be ways to protect your fertility before or during treatment.
Cardiac disorders
Radiation therapy to the chest and certain chemotherapy drugs, such as doxorubicin, can cause damage to the heart. Heart conditions that can occur include the following:
inflammation of the protective sac around the heart (pericarditis)
narrowing or blockage of the blood vessels in the heart (coronary artery disease)
scarring or weakening of the heart muscle (cardiomyopathy)
accumulation of fluid in the sac around the heart (pericardial effusion)
Weakened heart muscle (congestive heart failure) or an irregular heartbeat can cause shortness of breath and swelling in the hands or feet.
Your healthcare team will take steps to prevent, find, and treat these heart problems.
Lung disorders
Some chemotherapy drugs, such as bleomycin, can cause damage to the lungs. Radiation therapy to the lungs can also damage them. Lung disorders include these:
- inflammation of the lungs (pneumonitis)
- scarring or hardening of lung tissue (pulmonary fibrosis)
Radiation lung usually appears 1 to 3 months after starting radiation therapy, but it can also develop several months after treatment. Pulmonary fibrosis can develop months or even years after radiation therapy. These problems can cause coughing or shortness of breath.
Secondary cancers
In rare cases, a different type of cancer can form after treatment for HL. Breast cancer, for example, is likely to develop in a young woman who has received radiation therapy to the chest. Lung cancer can occur in a person who smokes and receives radiation therapy to the chest. Acute myelogenous leukemia (AML) or myelodysplastic syndrome can affect a person who has had a stem cell transplant.
Although the possibility of getting a second cancer can be scary, the benefits of treating HL with chemotherapy or radiation therapy usually far outweigh the risk of getting another cancer. The occurrence of secondary cancer depends on the following factors:
- type of chemotherapeutic agents
- administered dose
- duration of treatment
- combination of chemotherapy and radiotherapy
You can help reduce your risk of getting secondary cancer by adopting a healthy lifestyle and working with your healthcare team to design a wellness plan to stay healthy. Routine screening for early detection of secondary cancers, as well as being aware of changes in your health and reporting any problems to your doctor, are also important components of post-cancer treatment follow-up.
Emotional health
In treatment, the goal is to get through this stage and it can be difficult to stay positive. Money, work and different relationships can be a source of worry and anxiety. After treatment, you may think of other things and experience unexpected emotions, including the following:
- reappearance of LH
- effects of HL on your family,
Lymphoma is group of blood cancers. Lymphoma is cancer of the lymphatic system at the expense of lymphocytes.
The lymphatic system includes the bone marrow, spleen, thymus gland, lymph nodes and lymphatic vessels; it defends the body against microbes, parasites, toxins, foreign bodies, etc.
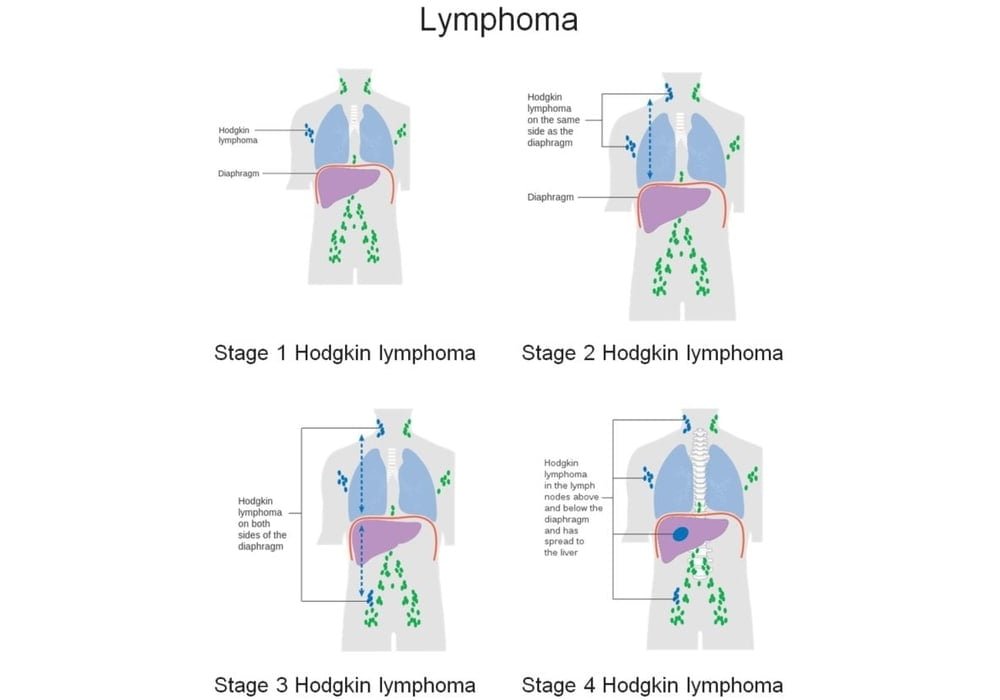
Stages of Hodgkin lymphoma
Staging describes the size of the lymphoma in the body and its location at the time of initial diagnosis. This is often referred to as the extent of lymphoma. The information from the tests is used to find out how big the tumor is, whether the lymphoma has spread from where it started and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The most frequently used staging systems for Hodgkin lymphoma (HL) are the Ann Arbor and Lugano staging systems. The systems are similar, and the one in Lugano is based on the Ann Arbor system. These two systems have 4 stages. For stages 1 to 4, the Roman numerals I, II, III and IV are often used. But in order to make the text clearer, we will use the Arabic numerals 1, 2, 3 and 4.
In general, the higher the stage number, the more the lymphoma has spread. Stages 1 and 2 are often considered early LH. Stages 3 and 4 correspond to advanced HL. Talk to your doctor if you have questions about staging.
Doctors determine the stage of HL after checking:
the number of groups of lymph nodes affected by the lymphoma;
if the lymphoma is localized or generalized – localized means cancerous lymph nodes are found in only 1 area of the body and generalized means cancerous lymph nodes are found in many areas of the body;
which lymph nodes are affected by lymphoma and whether they are on one or both sides of the diaphragm;
if the lymphoma is present in an organ or tissues other than the lymph nodes.
Categories A, B, E and X
The following letters can be added to the stage number depending on the aspect of the disease.
A – You don’t have a fever, you don’t sweat profusely, and you haven’t lost weight.
B – You have a fever, the cause of which is unknown and which does not go away, you have profuse night sweats and you have lost weight for no reason.
E – Lymphoma is found in neighboring tissue, outside the lymph nodes (extranodal seat).
X – Lymphoma occupies large areas (voluminous disease).
Stage 1
Lymphoma is found in 1 group of lymph nodes.
Stage 1E
Lymphoma is only found in 1 area outside the lymph nodes.
Stage 2
Lymphoma is found in at least 2 groups of lymph nodes. The lymph nodes affected by lymphoma are all located above or below the diaphragm.
Stage 2E
Lymphoma is found in the lymph nodes which are all above or below the diaphragm and it has also spread to the tissue near the nodes.
Stage 3
Lymphoma is found in the lymph nodes above and below the diaphragm.
Stage 3E
Lymphoma is found in the lymph nodes above and below the diaphragm and has also spread to the tissue near the nodes
Stage 4
Lymphoma is generalized: It is seen in areas of the body outside the lymph nodes such as the lungs, liver, bones and bone marrow. It is usually also seen in the lymph nodes.
LH relapse
Recurrence (relapse) of LH means that the lymphoma comes back after treatment. If it reappears where it first started, it is called a local recurrence. But it can reappear in another part of the body.
When LH comes back, it usually does so in the form it started. This means that low-grade (indolent) HL usually comes back as low-grade lymphoma. But sometimes a type of low-grade HL will come back as high-grade (aggressive) HL.
Refractory LH
LH is refractory when it has not responded to treatment. It is also called progressive disease.
If Hodgkin lymphoma spreads
Hodgkin lymphoma (HL) cells can spread from the lymph nodes where the cancer started to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer usually grows and spreads helps your healthcare team plan your treatment and future care. LH usually spreads in a predictable fashion, first invading the nearest lymph nodes. It is different from non-Hodgkin lymphoma (NHL), which does not spread in a predictable way.
IF LH spreads, it can spread to the following parts of the body:
- other groups of lymph nodes
- liver
- lung and pleura
- bone marrow
- bone
- skin
Prognosis and survival for Hodgkin lymphoma
If you have Hodgkin lymphoma (HL), you may be wondering about your prognosis. Prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many risk factors. Only a doctor who is familiar with your medical history, the type of cancer you have, the stage and characteristics of the disease, the treatments chosen, and the response to treatment can review all of this data together with survival statistics to determine if it is. arrive at a prognosis.
A prognostic factor is an aspect of cancer or a characteristic of the person that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. We often discuss prognostic and predictive factors together. They both play a role in choosing the treatment plan and in establishing the prognosis.
The stage of LH is an important factor in establishing the prognosis and planning treatment. However, the extent of LH spread and the organs or areas of tissue affected can vary within a single stage. Doctors therefore rely on the following factors to make a prognosis for early or advanced HL. These factors are called unfavorable or negative risks because they imply that the risk of reoccurrence (recurrence, or relapse) of LH after treatment is higher.
Early Hodgkin lymphoma
Early LH includes stages 1 and 2. Doctors determine whether early LH is favorable or unfavorable based on the following 5 factors. They may also use some of the International Prognostic Score (IPS) factors used for advanced HL. HL is favorable if none of these risk factors are present. LH is unfavorable if one or more of these risk factors are present.
Symptoms B
If a person has no B symptoms, doctors add the letter A after the stage. If she has any, they add the letter B. Early LH therefore includes stages 1A, 1B and 2A.
B symptoms are generalized, that is, they affect the whole body:
- unexplained fever
- profuse night sweats
- unexplained weight loss equivalent to more than 10% of body weight in the past 6 months
- Large mediastinal mass (thorax)
Chest tumors that are large, or bulky, often have a less favorable prognosis than small tumors because they tend to respond less well to treatment. Doctors may consider the following tumors to be large:
- chest tumor that is at least 1/3 the width of the chest on a chest x-ray
- tumor measuring at least 10 cm in diameter on computed tomography (CT)
Spread to areas other than lymph nodes
The prognosis for LH is more favorable if it is confined to the lymph nodes than if it has spread to other organs or areas of the body such as the bone marrow, liver or lungs. Doctors may name areas other than the lymph nodes as extranodal sites.
Spread to several lymph node regions
The prognosis for LH is less favorable if 3 or more lymph node regions are affected.
Globular sedimentation rate
The following red blood cell sedimentation rates (VSGs) are unfavorable risk factors:
- VSG greater than or equal to 50 mm / h in people who have no B symptoms
- VSG greater than or equal to 30 mm / h in people who experience B symptoms
Advanced Hodgkin lymphoma
Advanced LH includes stages 3 and 4. Some doctors also include people with B symptoms or people with large tumors.
The International Prognostic Score (IPS) helps doctors determine the prognosis and treatment of people with advanced HL. This is based on the following 7 unfavorable risk factors.
Stage 4
The prognosis of LH stage 4 is less favorable than that of LH stage 2B or 3.
Older age
The prognosis for people aged 45 or over is less favorable.
Male
The prognosis for men is less favorable than that of women.
Low hemoglobin level
A hemoglobin level below 105 g / L is less favorable.
Low albumin level
An albumin level of less than 40 g / L is less favorable.
High number of white blood cells
A number of white blood cells greater than or equal to 15,000 / mm3 is less favorable.
Low number of lymphocytes
A lymphocyte count less than 600 / mm3 or representing less than 8% of the total number of white blood cells is less favorable.
What is non-Hodgkin lymphoma?
Non-Hodgkin lymphoma (NHL) is a cancer that starts in lymphocytes. Lymphocytes are the cells of the lymphatic system.
The lymphatic system
The lymphatic system works in concert with other parts of your immune system to help your body defend itself against infection and disease. The lymphatic system is made up of a network of lymph vessels, lymph nodes and lymphatic organs. Lymph vessels carry lymph, which contains lymphocytes and other white blood cells, as well as antibodies and nutrients. Lymph nodes, which are located along the lymphatic vessels, filter lymph. Lymphatic organs include the spleen, thymus, tonsils, adenoids, and bone marrow.
Lymphocytes start in the bone marrow from basic cells called stem cells. Stem cells develop into different types of cells that have different jobs. Lymphocytes are a type of white blood cell that help fight infections. The main types of lymphocytes are:
B lymphocytes, or B cells, which produce antibodies to fight bacteria, viruses and other foreign substances such as fungi;
T lymphocytes, or T cells, which fight infections, destroy abnormal cells and control the immune response;
natural killer (NK) cells which attack abnormal or foreign cells.
Lymphocytes sometimes undergo changes that make the way they grow or behave abnormally. These abnormal cells can form tumors called lymphomas.
Since lymphocytes are found everywhere in the lymphatic system, NHL can manifest itself almost anywhere in the body. It usually appears in a group of lymph nodes in one part of the body, such as the neck (above the collarbone), under the arms, abdomen, or groin.
NHL can be spread to almost any tissue or organ in the body through the lymphatic system or the bloodstream. Abnormal lymphocytes, or lymphoma cells, can remain in the lymph nodes or form solid tumors. In rare cases, they circulate in the blood.
Types of NHL
There are over 30 different types of NHL. They are classified according to the kind of lymphocyte in which they develop. Most NHL begins in B cells and is called B cell lymphomas. They are also called B cell lymphomas or B lymphomas. NHL can also appear in T cells; it is then called T lymphoma, T cell lymphoma or T lymphoma. NHL that starts in NK cells is classified as T lymphoma.
Cells of different types of NHL do not all look the same under a microscope. In addition, they develop and spread in different ways. NHL is graded based on the appearance differences, or abnormalities, between lymphoma cells and normal lymphocytes. The grade gives doctors an idea of how quickly NHL could grow and spread. We usually classify NHLs in 2 grades:
Indolent, or low-grade, NHL has well-differentiated cancer cells, which means that they look and behave a lot like normal cells. This NHL tends to grow slowly.
Aggressive, or high-grade, NHL has poorly differentiated or undifferentiated cancer cells, that is, their appearance and behavior are less normal, or more abnormal. This NHL tends to grow quickly.
World Health Organization (WHO) classification system
Doctors use the WHO classification system to identify the type of NHL. Each type can behave differently and might require different treatments.
The WHO classifies NHLs according to the type of lymphocyte (B or T) that has become cancerous. NHL that starts in natural killer (NK) cells is classified as T-cell lymphoma.
The WHO then divides the B and T lymphomas into 2 groups based on the stage of development, or maturation, of the lymphocytes when they became cancerous. Precursor lymphoma develops in immature lymphocytes during the earliest stages of their development. Mature, or peripheral, lymphoma develops into more mature lymphocytes.
The specific type of NHL is based on the appearance of abnormal lymphocytes, or lymphoma cells, seen under a microscope, the characteristics of the chromosomes of lymphoma cells, and the presence of certain proteins on the surface of lymphoma cells.
WHO includes lymphomas and lymphoid leukemias as types of NHL: they both start in lymphocytes, but lymphoma cells are found in different places in the body. If the tumor appears in lymph nodes or other organs, it is considered lymphoma. If the lymphoma cells are in the blood or bone marrow and a tumor forms, it is said to be lymphoid leukemia.
Other cancers of the lymphatic system are called Hodgkin lymphoma (HL). The abnormal lymphocytes in Hodgkin lymphoma look and behave differently from those in non-Hodgkin lymphoma. These two categories of lymphoma are treated differently.
Diffuse large B cell lymphoma
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma (NHL). When viewed under a microscope, lymphoma cells look very large compared to normal lymphocytes. Lymphoma cells are also scattered throughout the lymph nodes and tissues.
DLBCL can appear in people of any age, but most are diagnosed when they are in their mid-sixties. It affects humans a little more often.
Usually, DLBCL starts in the lymph nodes, but it can also start in organs or tissues that are outside the lymph nodes (primary extranodal disease) and the most common locations include the following:
- bone
- brain or spinal cord (central nervous system, or CNS)
- digestive tract (gastrointestinal tract)
- sinus
- testicles
- thyroid gland
- skin
In 30 to 40% of cases, DLBCL is localized (stage 1 or 2) when diagnosed. The rest are prevalent at the time of diagnosis, which means that the DLBCL has spread to the lymph nodes above and below the diaphragm or to different parts of the body, such as the spleen, liver or bone marrow.
Rare subtypes of DLBCL include the following:
primary mediastinal large B cell lymphoma
primary serous lymphoma (LPS)
intravascular large B cell lymphoma
DLBCL is a rapidly growing (aggressive) type of NHL. Some types of slowly growing (indolent) B lymphoma can develop into DLBCL . These are among others:
follicular lymphoma
MALT lymphoma
lymphoma of the splenic marginal zone
small lymphocyte lymphoma
lymphoplasmacytic lymphoma
Symptoms
With DLBCL, the lymph nodes get bigger than normal, which is why they can be felt when touched. B symptoms, such as unexplained fever, heavy night sweats, and unexplained weight loss may also occur.
Treatments
DLBCL is very sensitive to chemotherapy, so it is used as the main treatment. Although DLBCL is a rapidly growing type of NHL, chemotherapy works for many people. It is possible that DLBCL will come back (recur) after the first few sessions of treatment are given.
Chemotherapy
Chemotherapy is used to treat all stages of DLBCL. The most common chemotherapy combination given as the initial treatment for DLBCL is called CHOP and is made up of the following drugs:
cyclophosphamide (Cytoxan, Procytox)
doxorubicin (Adriamycin)
vincristine (Oncovin)
prednisone
Chemotherapy is usually given with a targeted drug. This is referred to as the R-CHOP protocol, or the chemotherapeutic combination CHOP and rituximab (Rituxan).
If DLBCL comes back after being treated or if it does not respond to treatment, the following chemotherapy drugs should be given:
R-GDP – gemcitabine (Gemzar), dexamethasone (Decadron, Dexasone), cisplatin (Platinol AQ) and rituximab
R-DHAP – dexamethasone, cytarabine (Cytosar, Ara-C), cisplatin and rituximab
cytarabine
bendamustine (Treanda)
PEPC – prednisone, etoposide (Vepesid, VP-16), cyclophosphamide and procarbazine (Natulan)
R-ICE – ifosfamide (Ifex), carboplatin (Paraplatin, Paraplatin AQ), etoposide and rituximab
Targeted treatment
Targeted therapy uses drugs to target specific molecules (such as proteins) on the surface of cancer cells. These molecules help send signals that tell cells to grow or divide. By targeting these molecules, drugs stop the growth and spread of cancer cells while limiting damage to normal cells.
Rituximab is a targeted drug that is frequently used alone or in combination with chemotherapy to treat DLBCL.
Radiotherapy
External beam radiation therapy may be given after chemotherapy to treat stage 1 and sometimes stage 2 DLBCL. When DLBCL appears in one testicle, radiation therapy may be given to the other testicle as well to prevent further development. spread of lymphoma cells.
Radiation therapy may be given after chemotherapy in the presence of more advanced DLBCL. It is used if the disease is still present in a small area or if tumors measuring at least 10 cm in diameter are present in other areas (large disease).
Central nervous system prophylaxis
The central nervous system (CNS) is made up of the brain and the spinal cord. DLBCL that starts in the sinuses or testes can spread to the CNS. CNS prophylaxis is done to help prevent lymphoma cells from spreading to the brain and spinal cord.
CNS prophylaxis may be given by intrathecal chemotherapy, where the chemotherapy drug is injected directly into the cerebrospinal fluid (CSF). The drug used is methotrexate.
CNS prophylaxis can also be given with a needle inserted into a vein (intravenously). The drug used is high dose methotrexate.
Stem cell transplant
Other treatment options may be offered to people whose DLBCL does not go away after treatment or comes back after being treated (relapsed). These treatments may include other types of chemotherapy or a stem cell transplant. Stem cell transplantation may be an option if DLBCL has responded to chemotherapy before.
Immunotherapy
An immunotherapy called CAR T cell therapy may be offered to people with DLBCL that does not go away after treatment or that comes back after other treatments.
In CAR T cell therapy, millions of T cells are removed from a person with cancer. In the laboratory, they are modified so that they have chimeric antigen receptors (CARs) on their surface. These receptors recognize a specific antigen (protein) expressed by the type of cancer being treated. T cells are injected back into the person to multiply and then attack and destroy cancer cells.
Tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) are CAR T cell therapies approved as treatment for DLBCL that has come back after treatment (recurrence) or is unresponsive to treatment (refractory) after at least 2 more treatments. This includes DLBCL without further indication (NOS), high-grade B lymphoma, and DLBCL appearing in follicular lymphoma.
Follicular lymphoma
Follicular lymphoma is B-cell lymphoma. The word “follicular” refers to the way lymphoma cells cluster together in a lymph node or other tissue.
Follicular lymphoma is the 2nd most common type of non-Hodgkin lymphoma (NHL). It usually appears in adults 50 years of age or older, and the average age at diagnosis is 59 years. It affects women a bit more than men.
In most cases, follicular lymphoma is diagnosed at stage 3 or 4. It often spreads to the bone marrow and the spleen, but it usually does not affect other organs and tissues other than the lymph nodes.
Sometimes follicular lymphoma turns into diffuse large B cell lymphoma (DLBCL). DLBCL is a rapidly growing (aggressive) type of NHL.
Symptoms
Follicular lymphoma may not cause symptoms. Sometimes the lymph nodes in different parts of the body are larger than normal.
Prognostic factors
The healthcare team uses the Follicular Lymphoma International Prognostic Index (FLIPI) to help assess people with this disease and plan treatment. People with favorable prognostic factors should respond well to treatment. The risk of follicular lymphoma coming back (recurring) after treatment is higher when a person has poor prognostic factors.
| Prognostic factor | Good | Poor |
|---|---|---|
| age | 60 or younger | older than 60 |
| stage | 1 or 2 | 3 or 4 |
| hemoglobin | 120 g/L or higher | less than 120 g/L |
| number of lymph node areas that have lymphoma cells in them | 4 or less | more than 4 |
| lactate dehydrogenase (LDH) level | normal | higher than normal |
The healthcare team gives 1 point for each poor prognostic factor. They add up the points for a score of 0 to 5. People with good prognostic factors and a lower score have a better prognosis than those with 3 or more poor prognostic factors and higher scores.
Treatments
There are many treatment options for follicular lymphoma. This type of NHL often comes back (comes back) after being treated, but it usually responds to another course of treatment. The person often goes into remission again after being treated again, but remissions usually get shorter with each series of treatments.
Radiotherapy
External beam radiation therapy is used to treat lymph node regions affected by stage 1 or 2 follicular lymphoma. We can then speak of radiation therapy of the affected field.
Follicular lymphoma is usually more advanced (stage 3 or 4) and has usually spread to more than one lymph node area when diagnosed. Low dose external beam radiation therapy may be given to help relieve symptoms when follicular lymphoma is more advanced.
Vigilant observation
Watchful observation, also called active surveillance, may be suggested for follicular lymphoma because it grows slowly and may not need to be treated immediately. The healthcare team closely monitors the person with follicular lymphoma and begins treatment when symptoms appear or there are signs that the disease is progressing faster.
Chemotherapy
Chemotherapy may be offered to treat follicular lymphoma, especially if it has spread to several groups of lymph nodes or other organs and is causing symptoms. A single chemotherapeutic agent can be administered or a combination of several.
Chemotherapy is often combined with a targeted drug.
Only one of these drugs can be used:
- fludarabine (Fludara)
- bendamustine (Treanda)
- chlorambucil (Leukeran)
These drug combinations can be administered:
- CHOP – cyclophosphamide (Cytoxan, Procytox), doxorubicin (Adriamycin), vincristine (Oncovin) and prednisone
- R-CHOP – CHOP with rituximab (Rituxan)
- CVP – cyclophosphamide, vincristine and prednisone
- R-CVP – CVP with rituximab
- FND – fludarabine, mitoxantrone (Novantrone) and dexamethasone (Decadron, Dexasone)
- BR – bendamustine and rituximab
Targeted treatment
Targeted therapy uses drugs to target specific molecules (such as proteins) on the surface of cancer cells. These molecules help send signals that tell cells to grow or divide. By targeting these molecules, drugs stop the growth and spread of cancer cells while limiting damage to normal cells.
Rituximab is a targeted drug used to treat follicular lymphoma. It can be given on its own or in combination with chemotherapy. It can also be used as a maintenance treatment after chemotherapy.
There are other targeted drugs that can be used when follicular lymphoma comes back after being treated (comes back) or when it no longer responds to treatment, that is, the disease is refractory:
- ibritumomab (Zevalin)
- idelalisib (Zydelig)
- obinutuzumab (Gazyva) with bendamustine
Ibritumomab is a type of radioimmunotherapy, which binds radioactive material to the target drug. The targeted drug binds to lymphoma cells, causing radiation to be delivered directly to those cells, which may mean fewer side effects or less serious side effects.
Stem cell transplant
Stem cell transplantation may be an option for some people if follicular lymphoma comes back after treatment (comes back) or does not respond to treatment (refractory disease).
MALT lymphoma
Mucosal-associated lymphoid tissue lymphoma (MALT) of the extranodal marginal area is B-cell non-Hodgkin lymphoma (NHL). MALT lymphoma is said to be extranodal because it starts in tissues or organs outside the lymph node. lymph nodes. It appears in the lymphatic tissue of the mucous membranes or the tissue that lines organs or body cavities.
MALT lymphoma is also called maltoma. It affects men almost as much as women, usually in their 60s.
Most MALT lymphomas start in the stomach. More than 60% of people with MALT lymphoma of the stomach have a history of bacterial infection with Helicobacter pylori (H. pylori). Other bacterial and viral infections are also linked to MALT lymphoma.
People with MALT lymphoma in areas other than the stomach often have a history of autoimmune disorders such as Hashimoto’s thyroiditis and Sjögren’s syndrome. These areas of the body include the following:
- other parts of the digestive tract, such as the small intestine or the colon (the longest segment of the large intestine)
- lungs
- tissue around the eye
- skin
- salivary glands
- thyroid gland
- bladder
- breasts
In general, MALT lymphoma grows slowly (indolent), but sometimes it grows quickly (aggressive). It usually takes a long time to spread outside of the area where it started, and is often diagnosed at stage 1 or 2. Even if there are several extranodal sites, this does not mean that the lymphoma has spread. throughout the body (generalized disease).
In rare cases, MALT lymphoma can develop into a type of NHL that progresses quickly, that is, is aggressive.
Treatments
MALT lymphoma of the stomach is treated differently from MALT lymphoma that appears in another part of the body. Early-stage MALT lymphoma is often treated differently from advanced MALT lymphoma.
Early stage MALT lymphoma of the stomach
The treatment options for early stage MALT lymphoma (stage 1 or 2) that is confined to the stomach are as follows.
Antibiotics are often the first treatment if a biopsy confirms you have H. pylori infection. Antibiotics may be the only treatment needed if a follow-up biopsy shows the infection is gone and there is no sign of lymphoma.
Radiation therapy may be used if the antibiotics are not working. External beam radiation therapy is directed to tumors in the stomach.
Chemotherapy is sometimes given if the MALT lymphoma does not respond to antibiotics. Only one medicine, such as chlorambucil (Leukeran) or cyclophosphamide (Cytoxan, Procytox), can be used. Sometimes chemotherapy drugs are used together as in the case of the CHOP protocol, which is based on cyclophosphamide, doxorubicin (Adriamycin), vincristine (Oncovin) and prednisone.
Targeted therapy uses drugs to target specific molecules (such as proteins) on the surface of cancer cells. These molecules help send signals that tell cells to grow or divide. By targeting these molecules, drugs stop the growth and spread of cancer cells while limiting damage to normal cells. Rituximab (Rituxan) is a targeted drug that can be given if antibiotics are not working or if MALT lymphoma progresses after chemotherapy.
Surgery is sometimes done to remove part or all of the stomach (partial or total gastrectomy) if the lymphoma has not gone away after treatment with antibiotics or if it is progressing. Surgery is not done as much as before to treat MALT lymphoma of the stomach since other treatments are usually effective.
Early stage MALT lymphoma outside the stomach
Early-stage MALT lymphoma that has started in an area other than the stomach can be treated topically, such as with surgery or radiation therapy.
Surgery to remove the area affected by lymphoma may be an option depending on its location in the body and its size.
External beam radiation therapy can be given to the affected area.
Advanced MALT lymphoma
Advanced MALT lymphoma (stage 3 or 4) that is found in the stomach or another part of the body may be treated with any of the following treatments.
Vigilant observation, also called active surveillance, may be an option since MALT lymphoma grows slowly and may not need to be treated immediately. The healthcare team carefully monitors the person with MALT lymphoma and begins treatment. Especially when symptoms appear or there are signs that the disease is progressing.
Radiation therapy may be used if the lymphoma is large, is causing symptoms, or is growing. External beam radiation therapy is directed to the tumor and some of the surrounding tissue.
Chemotherapy may be used instead of radiation therapy if the lymphoma is large, if it gets bigger, if there is cancer all over the body (generalized disease), or if it comes back after being treated. The following drugs or drug combinations can be administered:
- fludarabine (Fludara)
- bendamustine (Treanda)
- chlorambucil (Leukeran)
CHOP protocol – cyclophosphamide (Cytoxan, Procytox), doxorubicin (Adriamycin), vincristine (Oncovin) and prednisone
CVP protocol – cyclophosphamide, vincristine and prednisone
Targeted therapy may be given if the MALT lymphoma of the stomach does not respond to antibiotics, if the lymphoma is not related to H. pylori infection, or if it comes back (comes back) after treatment. Rituximab (Rituxan) is a targeted drug that can be given on its own or in combination with chemotherapy.
Mantle cell lymphoma
Mantle cell lymphoma is a B-cell non-Hodgkin lymphoma (NHL). It starts in the outer edge of a lymph node called the mantle area. Mantle cell lymphoma affects men more often than women. It is usually diagnosed in your early sixties.
Usually mantle cell lymphoma is diagnosed at stage 3 or 4. It has often spread to other lymph nodes, bone marrow, spleen and liver. It is sometimes seen along the digestive tract (gastrointestinal tract). In this case, we can speak of lymphomatous polyposis.
Mantle cell lymphoma can grow slowly (indolent), but there are also rapidly growing (aggressive) variants called the blastoid variant and the polymorphic variant.
Treatments
The main treatment for mantle cell lymphoma is chemotherapy. Other treatments such as targeted therapy, biological therapy, radiation therapy and stem cell transplantation may be used.
Chemotherapy
Chemotherapy is frequently used to treat mantle cell lymphoma. Chemotherapy drugs are usually used in combination with a targeted drug sometimes added. The following chemotherapy combinations can be used:
- CHOP – cyclophosphamide (Cytoxan, Procytox), doxorubicin (Adriamycin), vincristine (Oncovin) and prednisone
- R-CHOP – CHOP with rituximab (Rituxan)
- CVP – cyclophosphamide, vincristine and prednisone
- R-CVP – CVP with rituximab
- hyper-CVAD – cyclophosphamide, vincristine, doxorubicin, dexamethasone (Decadron, Dexasone), methotrexate and cytarabine (Cytosar, Ara-C)
- R-hyper-CVAD – hyper-CVAD with rituximab
- EPOCH – etoposide (Vepesid), vincristine, doxorubicin, cyclophosphamide and prednisone
The following medicines may be used if mantle cell lymphoma does not respond to treatment, if it progresses during treatment, or if it comes back after treatment (comes back). It can be given as one or in combination with others or with a targeted drug:
- bendamustine (Treanda)
- cladribine (Leustatin)
- fludarabine (Fludara)
Targeted treatment
Targeted therapy uses drugs to target specific molecules (such as proteins) on the surface of cancer cells. These molecules help send signals that tell cells to grow or divide. By targeting these molecules, drugs stop the growth and spread of cancer cells while limiting damage to normal cells.
Rituximab (Rituxan) is a targeted drug that is frequently used alone or in combination with chemotherapy to treat mantle cell lymphoma.
Bortezomib (Velcade), ibrutinib (Imbruvica), and acalabrutinib (Calquence) are targeted drugs that are sometimes used to treat mantle cell lymphoma that comes back after being treated or stops responding to treatment.
Immunotherapy
Immunotherapy helps strengthen or restore the ability of the immune system to fight cancer. Lenalidomide (Revlimid) is the biological medicine that can be given for mantle cell lymphoma that comes back after being treated or stops responding to treatment.
Radiotherapy
External beam radiation therapy is sometimes used to treat mantle cell lymphoma. It can be given to affected lymph node areas when the disease is early on or to relieve symptoms (palliative treatment).
Stem cell transplant
Stem cell transplantation may be an option for some people who are in their first remission. It may also be used to treat mantle cell lymphoma that comes back after being treated or stops responding to treatment.
People with mantle cell lymphoma who cannot receive a stem cell transplant, or those whose cancer comes back after a stem cell transplant, may receive targeted therapy, biologic therapy, or another chemotherapy regimen.
Risk factors for non-Hodgkin lymphoma
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors, but sometimes non-Hodgkin lymphoma (NHL) develops in people who do not have any of the risk factors described below.
The risk of NHL increases with age. NHL is more common in people aged 60 and over. In general, NHL affects men more often than women, but specific types of NHL are more common in women.
Some people with specific genetic disorders are at higher than average risk of developing NHL. Discuss your risk with your doctor. If you have a genetic disorder that increases your risk of getting NHL, you may need to see your doctor more often to check for NHL. Your doctor will tell you which tests to take and how often.
The following are risk factors for NHL. Most of the risk factors cannot be changed. It means you can’t change them. Until we know more about these risk factors, there is no specific way to reduce your risk.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
Risk factors
Weakened immune system
Autoimmune disorders
Some infections
Treatment of cancer already given
Lindane exposure
Family history of NHL
Breast implants
There is convincing evidence that the following factors increase your risk for NHL.
Weakened immune system
A person with a weakened immune system is more likely to develop NHL. When you are born, your immune system may have already been damaged, called congenital immune deficiency. It can also be damaged over the course of your life, known as acquired immune deficiency. The time your immune system has been damaged does not change your risk for developing NHL.
The following factors can weaken your immune system.
Immunosuppressive drugs
Immunosuppressive drugs affect the immune system so that it does not respond as it normally would. These medicines are given after an organ transplant so that the immune system of the person receiving them does not attack the transplanted organ.
A person who takes immunosuppressive drugs after a solid organ transplant, such as a kidney, heart or liver, is more likely to develop NHL. A person who takes these drugs for another condition, such as rheumatoid arthritis, lupus, or inflammatory bowel disease, is also more likely to develop NHL. But its risk is lower than that of a person taking immunosuppressive drugs after an organ transplant.
HIV and AIDS
Someone who has HIV (human immunodeficiency virus) or has AIDS (acquired immune deficiency syndrome) is more likely to have certain types of NHL. This risk is reduced as drugs are developed to treat AIDS and HIV infection.
Immunodeficiency disorders
Immunodeficiency disorders affect the natural ability of the immune system to defend itself against infection. People with an immunodeficiency disorder often have infections, which can be serious or unusual. She is also at greater risk for certain types of cancer.
You can have an immunodeficiency disorder when you are born. This type of disorder is usually inherited, meaning that it is passed from parents to children. Immunodeficiency disorder can also start in your lifetime. It is said to be acquired. It can be caused by another disorder or a treatment that suppresses the immune system. Hereditary immunodeficiency disorders are very rare, but acquired ones are a little more common.
How NHL develops depends on the specific disorder and what part of the immune system it affects. The following immunodeficiency disorders increase your risk of developing NHL:
- ataxia telangiectasia (AT)
- Wiskott-Aldrich syndrome (SWA)
- variable-expression hypogammaglobulinemia (HGEV)
- severe combined immunodeficiency (SCID)
- X-linked lymphoproliferative syndrome (XLP)
Autoimmune disorders
Autoimmune disorder occurs when the immune system attacks tissues in the body. Some of these disorders have been linked to an increased risk of NHL. But only a small number of case of NHL are linked to autoimmune disorders.
The following autoimmune disorders are linked to NHL:
- Sjögren syndrome
- rheumatoid arthritis
- systemic lupus erythematosus (SLE, or lupus)
- celiac disease
- Hashimoto’s thyroiditis
Some infections
The following viral and bacterial infections can increase your risk for NHL. They can damage lymphocytes or constantly stimulate the immune system so that it does not work properly.
The Epstein-Barr virus (EBV) is a type of herpes virus that causes infectious mononucleosis, also called mono or kissing disease. EBV is linked to Burkitt’s lymphoma and NHL which affects people with weakened immune systems due to HIV or AIDS or immunosuppressive drugs. This virus and Burkitt’s lymphoma most often occur in Africa.
Human T-lymphotropic virus type 1 (HTLV-1) increases the risk of developing adult T cell lymphoma / leukemia. It is most commonly seen in southern Japan and the Caribbean.
Helicobacter pylori (H. pylori) is a type of bacteria that causes stomach ulcers and inflammation of the lining of the stomach called gastritis. It is linked to a type of lymphoma that affects the stomach called lymphoma of the lymphoid tissue associated with mucous membranes, or MALT lymphoma.
Human herpesvirus 8 (HHV-8) is also called Kaposi’s sarcoma herpesvirus (HVSK). It is linked to primary serous lymphoma, body cavity lymphoma and AIDS-related lymphoma.
The hepatitis C virus (HCV) is a virus that can cause inflammation of the liver called hepatitis. HCV infection increases the risk of diffuse large B cell lymphoma (DLBCL), splenic marginal zone lymphoma (LZMS), and lymphoplasmacytic lymphoma.
Campylobacter jejuni (C. jejuni) is a type of bacteria that can cause gastrointestinal (GI) infections. It is linked to lymphoma of the lymphoid tissue associated with mucous membranes, or MALT lymphoma.
Treatment of cancer already given
People who have received chemotherapy, with or without radiation therapy, to treat another type of cancer are more likely to develop NHL. This is especially true for those who have been treated for Hodgkin lymphoma. But the benefits of treating cancer usually far outweigh the risk of developing secondary cancer.
The risk of developing NHL is higher in the first 5 years after treatment. But people who have been treated for cancer are at greater risk of developing NHL for the rest of their lives.
Lindane exposure
Lindane is a type of insecticide. It is also present in very low doses in the treatment of lice and head mites, but it is only used after other treatments have not been effective. Studies show that exposure to lindane increases the risk of NHL.
Family history of NHL
A person whose first-degree relative (father, mother, brother, sister or child) has been diagnosed with NHL is more likely to have the disease.
Breast implants
Women who have breast implants (silicone or saline based) sometimes have a rare type of NHL called anaplastic large cell lymphoma associated with breast implants (LAGC-AIM). This lymphoma starts in the scar tissue that forms around the implant. Recent research shows that the risk is higher in women whose implants are textured rather than smooth. Health Canada has suspended the medical license for a brand of textured breast implant.
Possible risk factors
The following factors have been linked to NHL in some way, but there is insufficient evidence to suggest that they are risk factors. More research is needed to clarify the role of these factors in the development of NHL:
- exposure to pesticides
- exposure to trichlorethylene
- occupational exposures (farmers, hairdressers and barbers, welders and people working in certain industries such as rubber, printing and forestry)
- hepatitis B virus (HBV) infection
- obesity
- exposure to benzene
- taking tumor necrosis factor inhibitors for autoimmune disease
Reduce the risk of non-Hodgkin lymphoma
You can reduce your risk for non-Hodgkin lymphoma (NHL) by adopting the following behaviors.
Avoid exposure to pesticides
Lindane is an insecticide that increases your risk for NHL, and other pesticides may increase your risk as well. Prolonged exposure to pesticides should be avoided or reduced. Avoid using pesticides for cosmetic purposes. If you must use pesticides, use less. Follow your province’s occupational health and safety requirements, such as avoiding areas treated with pesticides for a period of time. Follow the directions on the product label for how to use pesticides safely. Wear the recommended protective clothing and equipment, such as gloves or a mask, when applying pesticides.
Have a healthy weight
Some studies have shown that obesity can increase your risk for NHL. You can reduce your risk by maintaining a healthy weight. Eating well and being physically active can help you maintain a healthy weight.
Follow workplace safety requirements
Working in certain industries, such as agriculture, rubber, lumber and forestry, printing and welding, can increase your risk for NHL. Specific occupational exposures, such as those to trichlorethylene, hair dyes and benzene, can also increase the risk of NHL. Follow workplace safety standards when working with hazardous chemicals.
Find out if your risk for NHL is high
Some people may be at higher than average risk for developing NHL. Discuss your risk with your doctor. If it is above average, you may need to see your doctor more often to check for NHL. Your doctor will tell you which tests to take and how often.
Diagnosis of non-Hodgkin lymphoma
The diagnostic process for non-Hodgkin lymphoma (NHL) usually begins with a visit to your family doctor. Your doctor will ask you about your symptoms and do a physical exam. Based on this information, your doctor may refer you to a specialist or order tests to check for the presence of NHL or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay to worry, but try to remember that other medical conditions can cause symptoms similar to NHL. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of NHL.
The following tests are commonly used to rule out or diagnose NHL. Many tests that can diagnose cancer are also used to determine its stage, that is, how far the disease has progressed. Your doctor may also give you other tests to check your general health and help plan your treatment.
Health history and physical examination
Your health history consists of a checkup of your symptoms, risk factors, and any medical events and conditions you may have had in the past. As you write down your health history, your doctor will ask you questions about your personal history:
- symptoms that suggest NHL
- medicines or conditions that could weaken your immune system
- immunosuppressive drugs after an organ transplant
- HIV / AIDS
- immunodeficiency disorders
- autoimmune disorders
- recent infections
- cancer treatment already given
- exposure to pesticides
Your doctor may also ask you if there is a history of NHL in your family.
The physical exam allows your doctor to look for any signs of NHL. During the physical exam, your doctor may:
feel the lymph nodes in your neck, armpits and groin to see if they are larger than normal (swollen);
feel your abdomen to see if your spleen or liver is larger than normal.
listen to your lungs;
check for signs of infection.
Biopsy
During a biopsy, the doctor removes tissue or cells from the body for analysis in a pathology laboratory. The laboratory report confirms the diagnosis and type of NHL.
The type of biopsy your doctor does depends on the location of the swollen lymph nodes. It can remove all or part of a lymph node in the neck, armpit or groin. They may also take a sample from a lymph node in the chest or abdomen. Computed tomography (CT) may be used as a guide for a lymph node biopsy in these areas.
NHL can appear in organs or tissues outside the lymph nodes (extranodal sites), including the brain, breast, skin, stomach, liver and intestine. The doctor may take biopsies to find out if NHL or another type of cancer is affecting these organs or tissues. Sometimes the doctor will take a biopsy of these organs or tissues to determine the stage of NHL.
Surgical biopsy
There are 2 types of surgical biopsy.
An excisional biopsy removes the entire lymph node or mass, along with a region of tissue around it.
An incisional biopsy takes a sample of tissue from a lymph node or other part of the body.
Drill biopsy
In a core biopsy, a hollow needle is used to take a sample from a lymph node or other part of the body.
Bone marrow puncture and biopsy
During a bone marrow puncture and biopsy, the doctor removes cells from the bone marrow to have them analyzed in the laboratory.
A doctor may use a bone marrow biopsy and puncture to diagnose NHL, but it is mostly used to determine the stage because it can spread to the bone marrow. The laboratory report confirms whether or not lymphoma cells are present in the sample.
Lumbar puncture
A lumbar puncture, or rachicentesis, is used to remove a small amount of cerebrospinal fluid (CSF) from the space around the spine that will be examined under a microscope. The CSF sample will show whether NHL is present in the brain and spinal cord (which together make up the central nervous system, or CNS). It is used to:
help diagnose primary CNS lymphoma;
find out if an NHL that started elsewhere in the body has spread to the CSF or the brain.
Cell and Tissue Studies
Cytogenetics is the analysis of a cell’s chromosomes, including their number, size, shape and arrangement. Cytogenetic techniques reveal chromosomal abnormalities, which helps doctors confirm the diagnosis and establish the type of NHL. The results of cytogenetic studies also help doctors plan treatment and predict how well it will work.
Significant chromosomal abnormalities can be detected by looking at cells under a microscope. But most changes in DNA require more careful analysis using other molecular techniques.
Fluorescence in situ hybridization (FISH)
Fluorescence in situ hybridization (FISH) is a molecular genetic test that identifies chromosomal abnormalities and other genetic changes in lymphoma cells. Special DNA probes labeled with fluorescent dyes are used. FISH is used to diagnose genetic abnormalities in different types of NHL, which can help doctors plan treatment.
Polymerase chain reaction (PCR)
Polymerase chain reaction (PCR) is used to make many copies of a particular segment of a gene for testing in the lab. Doctors use PCA to find changes in genes and certain changes in chromosomes that are too small to see under a microscope. It can help them diagnose a specific type of NHL and make a prognosis for it.
Immunophenotyping
Immunophenotyping is the study of proteins expressed by cells. It is used to determine the type of NHL.
Immunophenotyping is based on a very specific antigen-antibody reaction to identify proteins in tissues or cells. Monoclonal antibodies labeled with a fluorescent substance or a specific enzyme that bind only to specific antigens (proteins) are used. The fluorescent marker and the marker enzyme allow doctors to observe lymphoma cells.
The 2 methods which follow are the most used in immunophenotyping.
In immunohistochemistry, a microscope is used to observe fluorescent markers. It also allows doctors to examine cells and their surroundings.
Flow cytometry allows doctors to sort and classify cells using fluorescent markers on their surface. Doctors can see many antibodies all at once. The cells are exposed to a laser which causes them to emit light that is measured and analyzed by a computer. Flow cytometry can quickly collect data from thousands of cells present in a single sample.
Flow cytometry helps doctors define the unique characteristics of lymphoma cells. These characteristics can help doctors make a prognosis and measure response to treatment based on minimal residual disease (MRD). MRM refers to the presence of lymphoma cells in the bone marrow that cannot be found with standard laboratory tests.
Complete blood count
The complete blood count (CBC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. It is used for:
help rule out infection;
assess how well the organs that make blood, such as the bone marrow and the spleen, work
find out if lymphoma cells have spread to the blood
obtain reference values with which we can compare the results of the next CBC carried out during and after the treatment.
Blood biochemical analyzes
A blood chemistry test measures the level of chemicals in the blood. It makes it possible to evaluate the quality of functioning of certain organs and also to detect anomalies. Blood chemistry tests help establish the stage of NHL and include the following.
Higher than normal lactate dehydrogenase (LDH) levels may mean that NHL has spread to the liver. LDH levels are often higher in people with aggressive – that is, rapidly changing – type of NHL.
Higher than normal alanine aminotransferase (ALT) and aspartate transaminase (AST) levels may mean that NHL has spread to the liver.
A higher than normal level of alkaline phosphatase may mean that NHL has spread to the bones or to the liver.
Other blood tests
You may be tested for HIV, hepatitis B virus (HBV) and hepatitis C virus (HCV) if you are diagnosed with a certain type of NHL or whether certain treatments could be given to you. Infection with these viruses may affect your treatment.
Pulmonary radiography
In an x-ray, low-dose radiation is used to produce images of the body’s structures on film. A chest x-ray is used to find out if lymph nodes in the chest are swollen and if NHL has spread to the lungs.
Computed tomography (CT scan)
In a CT scan, special x-ray machines are used to produce 3-dimensional and cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the photos into detailed images.
CT is used to:
- assess swollen lymph nodes;
- examine organs in the chest, abdomen, pelvis and other areas of the body;
- monitor response to treatment as part of follow-up.
Magnetic resonance imaging (MRI)
In MRI, powerful magnetic forces and radio waves are used to produce cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the images into 3-dimensional snapshots.
MRI scans are used to check if NHL has spread to the brain or spinal cord. Doctors also use MRI to rule out or diagnose primary CNS lymphoma.
Ultrasound
In an ultrasound, high-frequency sound waves are used to produce images of body structures. She permits :
- check the spleen or liver for swelling or look for signs of NHL in these organs
- to check whether the testes are affected by NHL;
- doctors to remove tissue for a biopsy.
Bone scan
In a bone scan, radioactive materials that attach to the bones (radiopharmaceuticals) and a computer are used to create an image of the bones. A bone scan is used to find out if NHL has spread to the bones when a person experiences bone pain or when the blood alkaline phosphatase level is higher than normal.
Positron Emission Tomography (PET scan)
A positron emission tomography (PET) scan uses a radioactive material called a radiopharmaceutical to detect changes in the metabolic activity of body tissues. A computer analyzes patterns of radioactivity distribution and produces 3-dimensional, color images of the region under examination.
Doctors are still trying to figure out how best to use PET to help diagnose and stage NHL. PET can be used to:
- identify regions affected by NHL;
- help monitor response to treatment and find recurrences.
Histological classification of non-Hodgkin lymphoma (grading)
Knowing the grade gives your healthcare team an idea of how quickly non-Hodgkin lymphoma (NHL) can develop and how likely it is to spread. It helps him plan your treatment. The grade can also help the healthcare team predict how you might respond to treatment.
To determine the grade of NHL, the pathologist examines a sample taken from a lymph node or other tissue under a microscope. The grade is defined by the appearance and behavior of cancer cells compared to normal cells. The word differentiation is used to refer to how different cancer cells are.
The different types and subtypes of NHL are usually described as indolent (low grade, or slowly developing) or aggressive (high grade, or rapidly developing). Some subtypes of NHL cannot be easily classified because they have characteristics of indolent NHL and aggressive NHL.
Low grade, or indolent NHL
Low-grade, or indolent, cancer cells are well differentiated. They look and behave very much like normal cells.
Low-grade types of NHL tend to grow slowly and usually cause few symptoms when they develop. Low-grade types of NHL have therefore often already spread to other parts of the body when diagnosed. Usually, they spread to the bone marrow and the spleen.
Certain types of low-grade NHL can develop into a high-grade type of NHL that requires more aggressive treatment.
High grade, or aggressive NHL
High-grade, or aggressive, cancer cells are poorly differentiated or undifferentiated. Their appearance and behavior are less normal, or more abnormal.
High-grade types of NHL grow quickly. They tend to spread to the lymph nodes or other organs in different parts of the body. High-grade types of NHL usually cause symptoms and should be treated immediately.
Stages of non-Hodgkin lymphoma
Staging describes the size of the lymphoma in the body and its location at the time of initial diagnosis. This is often referred to as the extent of lymphoma. The information from the tests is used to find out how big the tumor is, whether the lymphoma has spread from where it started and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The most frequently used staging systems for non-Hodgkin lymphoma (NHL) are the Ann Arbor and Lugano staging systems. The systems are similar, and the one in Lugano is based on the Ann Arbor system. These two systems have 4 stages. For stages 1 to 4, the Roman numerals I, II, III and IV are often used. But in order to make the text clearer, we will use the Arabic numerals 1, 2, 3 and 4. In general, the higher the stage number, the more the lymphoma has spread. Talk to your doctor if you have questions about staging.
Doctors determine the stage of an NHL after checking:
- the number of groups of lymph nodes affected by the lymphoma;
- which lymph nodes are affected by lymphoma and whether they are on one or both sides of the diaphragm;
- if the lymphoma is present in an organ or tissues other than the lymph nodes;
- if the lymphoma has spread to the same area of the body or further.
Categories A, B, E, S and X
You can also divide the NHL into categories, and you can add the following letters to the stadium number.
A – You don’t have a fever, you don’t sweat profusely, and you haven’t lost weight.
B – You have a fever, the cause of which is unknown and which does not go away, you have profuse night sweats and you have lost weight for no reason.
E – Lymphoma is found in neighboring tissue, outside the lymph nodes (extranodal seat).
S – The lymphoma has spread to the spleen.
X – Lymphoma occupies large areas (voluminous disease).
Stage 1
Lymphoma is found in 1 group of lymph nodes.
Stage 1E
Lymphoma is only found in 1 area outside the lymph nodes.
Stage 2
Lymphoma is found in at least 2 groups of lymph nodes. The lymph nodes affected by lymphoma are all located above or below the diaphragm.
Stage 2E
Lymphoma is found in the lymph nodes which are all located above or below the diaphragm. The lymphoma has also spread to the tissue near the lymph nodes.
Stage 3
Lymphoma is found in the lymph nodes above and below the diaphragm.
Stage 3S
Lymphoma is found in the spleen and lymph nodes above the diaphragm.
Stage 4
Lymphoma is generalized: It is seen in multiple areas of the body such as the lungs, liver, bones, bone marrow or cerebrospinal fluid (CSF). It is usually also seen in the lymph nodes.
NHL recurrence
A recurrence of NHL means that the lymphoma comes back after treatment. If it reappears where it first started, it is called a local recurrence. But it can reappear in another part of the body.
When NHL comes back, it usually does so in the form it started. This means that low-grade (indolent) NHL usually comes back as low-grade lymphoma. But sometimes a low-grade type of NHL will come back as a high-grade (aggressive) NHL.
Refractory NHL
NHL is refractory when it has not responded to treatment. It is also called progressive disease.
Spread of non-Hodgkin lymphoma
Understanding how a type of cancer usually grows and spreads helps your healthcare team plan your treatment and future care. Non-Hodgkin lymphoma (NHL) can spread through the lymphatic system, and sometimes through the bloodstream, to almost any tissue or organ in the body.
NHL usually starts in an area of lymph nodes. When it spreads to an organ or tissue outside the lymph nodes, it is called extranodal spread.
IF NHL spreads, it can do so in the following structures:
- other lymph nodes near the original site or in other parts of the body
- bone marrow
- liver
- stomach
- small intestine
- large intestine
- lung or pleura
- testicles
- brain or spinal cord (which together make up the central nervous system, or CNS)
- skin
- eyes
- sinus
Indolent (low grade) types of NHL have often already spread to different parts of the body when diagnosed. Lymphoma cells can be found in many lymph nodes, bone marrow or spleen.
Aggressive (high grade) types of NHL have usually not yet spread outside the lymph node region or the organ in which they originated when diagnosed.
NHL processed
Some indolent types of NHL can develop into a more aggressive type of NHL, usually diffuse large B-cell lymphoma (DLBCL). The indolent types of NHL that can transform include the following:
- follicular lymphoma
- chronic lymphocytic leukemia and small lymphocyte lymphoma
- marginal zone lymphoma
Prognosis and survival for non-Hodgkin lymphoma
If you have non-Hodgkin lymphoma (NHL), you may be wondering about your prognosis. A prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your health history, the type of cancer you have, the stage and characteristics of the disease, the treatments chosen and the response to treatment can review all of this data together with the survival statistics for. come to a prognosis.
A prognostic factor is an aspect of cancer or a characteristic of the person that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. Prognostic and predictor factors are often discussed together and both play a role in choosing a treatment plan and establishing the prognosis.
Revised international prognostic index
The Revised International Prognostic Index (RIPI) is a more recent version of the International Prognostic Index (IPI) that has been developed to help determine the outcome of people with aggressive (rapidly progressing) type of NHL .
RIPI is based on treatments with brand new drugs including rituximab (Rituxan). It helps doctors assign risk categories to people with the condition based on the number of adverse prognostic factors they have. RIPI uses the same factors as IPI and divides people into 3 risk categories.
Age
People under the age of 60 tend to have a better prognosis than those over the age of 60.
Stadium
The lower the stage of NHL, the better the prognosis. Stage 1 or 2 NHLs have a more favorable prognosis than stage 3 or 4 NHLs.
Lacticodehydrogenase (LDH) level
A person with normal LDH levels in their blood tends to have a better prognosis than a person with high LDH levels. A higher than normal LDH level usually means that the cancer is more advanced. LDH levels are often higher in people with a rapidly changing type of NHL.
Extranodal spread
When NHL spreads to an organ or tissue outside the lymph nodes, it is called extranodal spread. An NHL that is only found in the lymph nodes is more likely to be treated effectively and has a better prognosis than an NHL that has spread outside the lymph nodes.
Functional index
The Functional Index is a measure of a person’s ability to perform routine tasks as well as their daily activities. In general, the more active a person is and the better able they are to carry on with their daily activities, the better the Functional Index. People with a good functional index, i.e. those who can function almost normally, usually have a better prognosis than those with a low functional index, i.e. those who need help with their activities. daily or who have to spend a lot of time in bed.
RIPI Risk Categories
Doctors assign the prognostic score based on the RIPI. One point is allocated to each unfavorable prognostic factor. The lower the number of adverse prognostic factors, the better the prognosis.
A very good prognosis is not linked to any unfavorable prognostic factor.
A good prognosis is linked to 1 or 2 unfavorable prognostic factors.
A poor prognosis is linked to 3 or more unfavorable prognostic factors.
Doctors use RIPI to identify cases of NHL that are likely to respond well to treatment and those that are likely to come back (come back) after treatment.
Other prognostic factors
Doctors also take the following factors into consideration when assessing the prognosis for NHL.
Type of NHL
People with B-cell lymphoma often have a better prognosis than those with T-cell lymphoma. Of the 2 most common types of B-cell lymphoma, follicular lymphoma generally has a better prognosis than diffuse large B cell lymphoma (DLBCL). Anaplastic large cell lymphoma and cutaneous T lymphoma are 2 subtypes of T cell lymphoma that have a fairly good prognosis.
Tumor volume
The smaller the tumor, the better the prognosis. Small tumors tend to respond better to treatment. Large tumors often have a less favorable prognosis. A very large tumor (10 cm or more) may be called a large tumor.
Symptoms B
The symptoms B include unexplained fever, heavy night sweats, and unexplained weight loss. If B symptoms are present, the prognosis is less favorable.
Hemoglobin level
A person with a normal hemoglobin level has a better prognosis than a person with a low hemoglobin level.
Treatments for non-Hodgkin lymphoma
If you have non-Hodgkin lymphoma (NHL), your healthcare team will create a treatment plan just for you. It will be based on your needs and specific cancer information. When your healthcare team decides what treatments to offer you for NHL, they consider the following:
- the type of NHL
- the stage of cancer
- the grade of the cancer – indolent (low-grade, or slow-growing) or aggressive (high-grade, or fast-growing) NHL
- your prognostic factors
- your age
- your overall health
- previous administration of treatment for NHL
You may be offered a combination of the following treatments for NHL.
Chemotherapy
The chemotherapy drugs used depend on the type of NHL and its stage. You may be given one or a combination of chemotherapy drugs. High dose chemotherapy is used in preparation for a stem cell transplant.
Immunotherapy
Immunotherapy may be given alone or in combination with chemotherapy to treat certain types of NHL.
Targeted treatment
Targeted drugs may be given only or combined with chemotherapy to treat certain types of NHL. A few targeted drugs deliver radiation directly to lymphoma cells. This treatment is called radioimmunotherapy.
Radiotherapy
External beam radiation therapy may only be used as the main treatment for certain types of early stage NHL that have not spread to different parts of the body. It can also be combined with chemotherapy to treat aggressive or more advanced NHL.
Sometimes whole body external beam radiation therapy (total body radiation) is given in preparation for a stem cell transplant. It can also be given to the brain (commonly called the brain) to stop NHL from spreading to the central nervous system (CNS) or to treat NHL in the CNS.
Doctors may use radiation therapy to reduce the size of the tumor or larger than normal lymph nodes that put pressure on nerves, causing pain. Giving radiation therapy to these areas can help reduce the size of large tumors and relieve pain.
Vigilant observation
Vigilant observation is also called active surveillance. It may be an option for some indolent types of NHL that are not yet causing symptoms. The healthcare team is watching carefully for signs that indicate that the NHL is progressing. She starts treatment if the disease progresses and causes symptoms.
Active Cancer Surveillance and Visits | Monitoring and Follow-up for Cancer Survivors
Surgery
Surgery is mostly used to remove part or all of a lymph node to diagnose NHL. Sometimes surgery is done to remove the spleen (splenectomy). In some cases, surgery may be used to remove the entire tumor if it has not invaded nearby tissues or organs.
Stem cell transplant
A stem cell transplant may be used to treat some people at high risk of recurrence and who are in remission. A stem cell transplant can also be done to treat NHL that comes back (comes back) after being treated or that no longer responds to treatment.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits. They are usually scheduled every two months for the first year or more, then gradually you will see doctors less and less often. These visits allow the healthcare team to monitor your progress and to know how you are recovering from treatment.
Clinical tests
A few clinical trials for NHL are available in some countries and are accepting participants. Clinical trials aim to find new and better methods of cancer prevention, detection and treatment.
Follow-up after treatment for non-Hodgkin lymphoma
Follow-up after treatment for non-Hodgkin lymphoma (NHL) is an important part of caring for people with the disease. Cancer specialists (oncologists) and your family doctor often share this responsibility. Your healthcare team will talk to you to decide which follow-up meets your needs.
Don’t wait until your next scheduled appointment to report any new symptoms and any symptoms that don’t go away. Tell your healthcare team if you have the following symptoms:
- new lump or swelling
- fever that persists
- night sweats
- weight loss that happens for no reason
Planning of follow-up visits
Follow-up visits for NHL are usually scheduled on a regular basis every 2 months, at least for the first year after treatment, and then gradually less often.
In rapidly progressing (aggressive) lymphoma, follow-up visits are quite often during the first 3 years after treatment and less frequently thereafter. There are very few recurrences 5 years after treatment for aggressive lymphoma, so regular visits may not continue beyond this time.
In slow-onset (indolent) lymphoma, regular follow-up visits usually continue throughout the person’s life.
Progress of follow-up visits
During a follow-up visit, your healthcare team will usually ask you questions about the side effects of treatment and how well you are coping. You may also be asked if you are experiencing any new symptoms and if your vaccines are up to date.
Your doctor may do a physical exam, including:
- take your vital signs to see if there is a fever, shortness of breath or a fast heartbeat
- check by palpation if the lymph nodes in your neck, armpits and groin are swollen;
- feel your abdomen to see if any organs are swollen;
- examine your bones to see if they are tender or painful.
Examinations are often ordered as part of the follow-up. We can ask for these:
- complete blood count (CBC) to check for abnormal blood cell counts
- blood chemistry tests to assess how well certain organs are working
- imaging tests, such as a chest x-ray, computed tomography (CT), magnetic resonance imaging (MRI), or
- ultrasound, to get useful information about the spleen, liver, or lymph nodes
- bone marrow puncture and biopsy for further evaluation after getting blood test results or if new symptoms appear
If there is a recurrence at follow-up, your healthcare team will assess you to determine the best treatment options.
Supportive care for non-Hodgkin lymphoma
Self-esteem and body image
Tired
Infections
Fertility disorders
Cardiac disorders
Thyroid gland disorders
Lung disorders
Secondary cancers
Emotional health
Supportive care empowers people to overcome the physical, practical, emotional and spiritual barriers of non-Hodgkin lymphoma (NHL). It is an important component of the care of people with this disease. There are many programs and services that help meet the needs and improve the quality of life for these people and their loved ones, especially after treatment is over.
Recovering from NHL and getting used to life after treatment is different for everyone. Recovery depends on the stage and grade of the disease, the type of treatment given, and many other factors. The end of cancer treatment can lead to mixed emotions. Even if the treatment is finished, there may be other issues that need to be addressed, such as coping with long-term side effects.
Someone who has been treated for NHL may be concerned about the following.
Self-esteem and body image
Self-esteem is how you feel about yourself or how you see yourself. Body image is how we perceive our own body. NHL and its treatments can affect self-esteem and body image. This is often because cancer or cancer treatments cause changes in the body such as the following:
- hair loss
- skin changes
- changes in body weight
Some of these changes may be temporary. Others will last a long time and some will be permanent.
Tired
Fatigue is a symptom of a low number of red blood cells (anemia). Red blood cell counts may be low when the bone marrow is affected by NHL or its treatments. Fatigue can also be a symptom of other problems that people with NHL may have, including malnutrition, sleep disturbances, anxiety and depression.
Once the cause of fatigue is known, your healthcare team can suggest ways to deal with it:
- iron pills if your iron levels are low
- blood transfusion for anemia
- nutritional supplements
- sleeping tablets
- antidepressants
Infections
An infection can happen if your white blood cell count is low (neutropenia). The number of white blood cells may be low when NHL or its treatments affect the bone marrow.
Preventing infections is important for people with NHL. Practicing good hygiene, protecting your skin, and maintaining good overall health are some of the ways you can help prevent infections. It is also important to keep your vaccines up to date to help prevent certain infections.
Your healthcare team can give you medicine to prevent infections if your white blood cell count is low. You will also be given medicines to treat infections such as antibiotics, antivirals, and antifungals.
Fertility disorders
Some treatments for NHL can cause fertility problems in both men and women. These problems can include infertility, which is the inability to conceive a child. The onset of infertility depends on the type of treatment and the area of the body being treated. Combinations of chemotherapy drugs and radiation therapy to the pelvis and surrounding areas can cause fertility problems.
Women treated for NHL who are naturally approaching menopause are the most likely to become infertile since treatment can cause early menopause. Younger women treated for NHL may experience symptoms of menopause and become temporarily infertile. They have a better chance than older women to become fertile again.
Some treatments can make a man temporarily or permanently infertile if they reduce or interrupt the production of sperm in the testes.
Discuss your fertility with your healthcare team before treatment begins.
Cardiac disorders
Radiation therapy to the chest and certain chemotherapy drugs can cause damage to the heart. Heart conditions that can occur include the following:
- inflammation of the surrounding protective bag the heart (pericarditis)
- narrowing or blockage of the blood vessels in the heart (coronary artery disease)
- scarring or weakening of the heart muscle (cardiomyopathy)
- accumulation of fluid in the sac around the heart (pericardial effusion)
Weakened heart muscle (congestive heart failure) or an irregular heartbeat can cause shortness of breath and swelling in the hands or feet.
Your healthcare team will take steps to prevent, find, and treat these heart problems.
Thyroid gland disorders
People who receive radiation therapy to the neck as treatment for NHL are more likely to develop hypothyroidism later on. Hypothyroidism is the insufficient production of thyroid hormone by the thyroid gland, which interferes with the normal functioning of the body. It usually appears 3 to 4 years after radiation therapy, but it can also appear later.
The healthcare team regularly checks the function of the thyroid gland. Some people need to take thyroid hormone replacement therapy to regulate their thyroid gland.
Lung disorders
Radiation therapy to the chest can damage the lungs. Lung disorders that can occur include the following:
- inflammation of the lungs (pneumonitis)
- scarring or hardening of lung tissue (pulmonary fibrosis)
Radiation lung usually appears 1 to 3 months after starting radiation therapy, but it can also develop several months after treatment. Pulmonary fibrosis can develop months or even years after radiation therapy. These problems can cause coughing and shortness of breath.
Secondary cancers
In rare cases, a different type of cancer can form after treatment for NHL. Breast cancer, for example, is likely to develop in a young woman who has received radiation therapy to the chest. Lung cancer can occur in a person who smokes and receives radiation therapy to the chest. Acute leukemia or myelodysplastic syndrome can affect a person who has had a stem cell transplant.
Although the possibility of having a second cancer can be scary, the benefits of treating NHL with chemotherapy or radiation therapy usually far outweigh the risk of developing another cancer. The occurrence of secondary cancer depends on the following factors:
- type of chemotherapeutic agents
- administered dose
- duration of treatment
- combination of chemotherapy and radiotherapy
Following the usual follow-up to detect secondary cancer early as well as being aware of changes that affect your health and reporting any problems to your doctor are important components of follow-up after cancer treatment.
Emotional health
In treatment, the goal is to get through this stage and it can be difficult to stay positive. Money, work and different relationships can be a source of worry and anxiety. After treatment, you may think of other things and experience unexpected emotions, including the following:
- reappearance of NHL
- effects of the NHL on your family, friends and career
- self-esteem and identity
- changes in your appearance
- adaptation to changes that affect your lifestyle
- anxiety about less contact with the healthcare team
Discuss your concerns with your healthcare team.
They can support you and help you adjust to the NHL in a number of ways including:
- engaging in appropriate physical activities
- feed you well
- balance between activity and rest
- speak openly and frankly about your fears and concerns
- find the right support and treatment if you are having emotional problems, such as counseling or taking medication
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, American Cancer Society, Web MD, Cancer Center, Cleveland Clinic
Photo credit: Wikimedia Commons 1, 2, 3, 4
Photo explanations: Diagram showing stage 1 to 4 Hodgkin’s lymphomas.