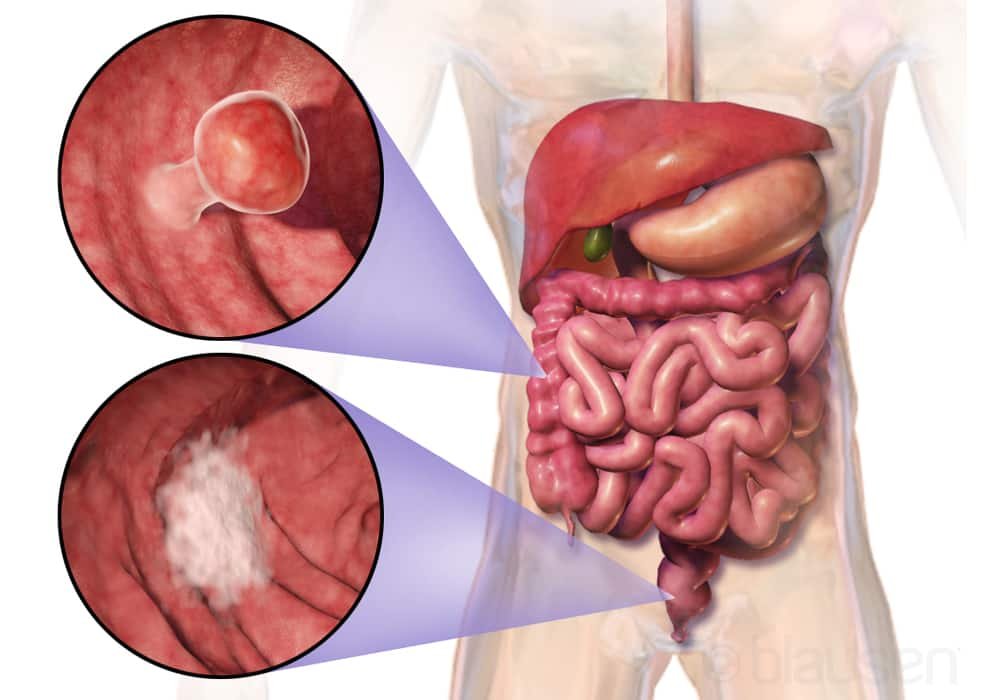
Colon Cancer (Colorectal)
Colorectal cancer is a malignant tumor starts in the colon or the rectum. Colorectal cancer can affect all anatomical segments of the large intestine such as the cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum but does not affect anal canal cancer which is a separate entity.
Colon cancer and rectal cancer are grouped together under the name of colorectal cancer. They develop from cells that line the inner wall of the colon or rectum, primarily by gradual transformation of a benign polyp.
The colon and rectum are part of the large intestine and the digestive system. The colon absorbs water and nutrients and passes waste products (stool, or feces) into the rectum. Cancers of the colon and rectum are grouped together under the category of colorectal cancer since these organs are made of the same tissues and there is no clear line between them.
Find out the basics about this digestive cancer, whose treatment success depends largely on the early diagnosis. This artical may help you to identify the symptoms that should alert you.
Symptoms of colon cancer
- the occurrence of abdominal pain;
- the presence of blood in the stool;
- sudden or worsening constipation;
- diarrhea that is prolonged;
- an alternation between diarrhea and constipation;
- a constant urge to have a bowel movement;
- a mass on palpation of the abdomen;
- unexplained deterioration in general condition, manifested in particular by loss of weight and appetite, reduction
- in food intake and fatigue;
- unexplained anemia.
Colon cancer may also be suspected if the stool blood test performed as part of the organized screening for colorectal cancer is positive.
What causes colon cancer
Age increases the risk of developing colon cancer: 9 out of 10 people with colon cancer are over 50 years old.
Lifestyle habits are also involved:
- a diet that is too rich, especially in animal fats;
- a significant consumption of red meats;
- physical inactivity;
- overweight ;
- Alcohol consumption ;
- tobacco consumption.
PERSONAL AND FAMILY HISTORY
The risk of developing colon cancer is increased in people with chronic inflammatory bowel diseases (such as Crohn’s disease and ulcerative colitis), genetic diseases (familial adenomatous polyposis), and Lynch syndrome (or HNPCC) ).
A family history of colon or rectal cancer is also a risk factor.
Genetic predisposition to colorectal cancers
In some cases, a genetic alteration (also called genetic variation), inherited from a parent, is present from birth in all cells of the body. It can then play a role in the development of cancer. We speak of a genetic predisposition to cancer, linked to the presence of what is called “a constitutional genetic alteration”.
If the doctors who follow you suspect a genetic predisposition to colorectal cancer, they will refer you to an oncogeneticist who will do a constitutional analysis of your genes.
If the tests reveal a hereditary genetic abnormality, a screening test may be offered to your brothers, sisters, parents or adult children (that is to say your first degree relatives). This test will determine if they are also carriers.
Risk factors for colon cancer
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors, but colorectal cancer can develop in people who do not have any of the risk factors described below.
Most people diagnosed with colorectal cancer are over 50, and the risk increases with age. More men than women have this type of cancer. The incidence rate for colorectal cancer is highest in North America, northwestern Europe and Australia. In less industrialized countries, especially in Asia, Africa and South America, the rate is lower.
Precancerous conditions of the colon or rectum include adenomas and hereditary colorectal cancer syndromes. These conditions are not cancerous, but they can turn into colorectal cancer if left untreated. Certain risk factors for colorectal cancer can also cause these precancerous conditions. Find out more about precancerous conditions of the colon or rectum.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
Risk factors:
- Family history of colorectal cancer
- Personal history of colorectal cancer
- Familial adenomatous polyposis (FAP)
- Lynch Syndrome
- Polyps in the colon and rectum
- Rare genetic disorders
- Physical inactivity
- Overweight or obese
- Alcohol
- Smoking tobacco
- Diet rich in red meat
- Processed meats
- Low fiber diet
- Sedentary behavior
- Inflammatory bowel disease (IBD)
- Diabetes
- Ashkenazi Jewish descent
- Personal history of breast, ovarian or uterine cancer
- Tall adult height
- Cooking meat at high temperature
- Exposure to ionizing radiation
There is convincing evidence that the following factors increase your risk for colorectal cancer.
Family history of colorectal cancer
When there is a family history of colorectal cancer, it is because one or more close blood relatives have or have had colorectal cancer. In some families, there are more cases of colorectal cancer than you might expect. Sometimes it is not clear whether this family disposition is due to chance, to a way of life that members of the family have in common, to a hereditary factor which has been transmitted from parents to their children through genes, or to a association of these elements.
In families where colorectal cancer is present, the risk is increased if:
A first-degree relative (such as father or mother, sibling or child) has had colorectal cancer in the past. The risk is further increased if the first-degree family member has had colon cancer rather than cancer of the rectum.
More than one first-degree relative has suffered from colorectal cancer.
A family member under the age of 50 was diagnosed with colorectal cancer.
Personal history of colorectal cancer
If you have ever had colorectal cancer, you are more likely to get a second colorectal cancer.
Familial adenomatous polyposis (FAP)
FAP is a rare inherited condition usually caused by a mutation in the colonic adenomatous polyposis (APC) gene. FAP is characterized by the formation of hundreds or thousands of adenomatous polyps on the inner lining (mucosa) of the colon and rectum. These polyps can appear as early as adolescence. If FAP is not treated, the majority of people who have it will develop colorectal cancer by the age of 40.
Attenuated familial adenomatous polyposis (attenuated PAF) is a subtype of PAF. People with attenuated PAF have fewer adenomatous polyps in the colon than those with classical PAF, and these polyps tend to appear later in life. Colorectal cancer usually shows up in people with milder PAF when they are older.
Lynch Syndrome
Also called hereditary nonpolyposis colorectal cancer or HNPCC, Lynch syndrome is an inherited condition caused by mutations in genes that correct any mistakes cells make when they divide and DNA is copied. It causes polyps to form in the lining of the colon, rectum, or both, but not as many as with PAF. Lynch syndrome is suspected when a person in their mid-forties has colorectal cancer or when some of their loved ones have been diagnosed have colorectal cancer at about this age.
There are 2 types of Lynch syndrome:
Type A (Lynch syndrome type 1) only increases the risk of colorectal cancer.
Type B (Lynch syndrome type 2) increases the risk of colorectal cancer as well as cancers of the stomach, small intestine, pancreas, kidney, ureter, ovary, cancer of the stomach. uterus, breast, bladder, bile ducts and skin.
Polyps in the colon and rectum
Having a personal or family history of polyps in the colon, rectum, or both, greatly increases the risk of colorectal cancer. Colorectal polyps usually form in the inner lining (lining) of the colon or rectum. Adenomas (adenomatous polyps) are polyps that can become cancerous.
The risk of colorectal cancer starting in adenomatous polyps is related to the type, size and number of polyps:
Tubular polyps are common, but they are usually smaller and less likely to become cancerous. Villous polyps are less common but are more likely to become cancerous.
Polyps larger than 1 cm are more likely to be cancerous.
The more polyps there are, the more likely it is that one of the polyps will become cancerous.
Rare genetic disorders
The rare genetic disorders described below can increase your risk of developing colorectal cancer.
Turcot syndrome is a variant of Lynch syndrome and PAF. Turcot syndrome is characterized by the presence of many polyps in the colon, which can become cancerous.
MYH-associated polyposis is caused by a mutation in the DNA repair gene called MUTYH. People with MYH-associated polyposis have many adenomatous polyps on the lining (lining) of the colon.
Juvenile polyposis syndrome is an inherited condition that causes polyps called hamartomas to form. Hamartomas are usually noncancerous, but they can become cancerous.
Peutz-Jeghers syndrome is an inherited condition that involves mutation of the STK11 gene. People with Peutz-Jeghers syndrome often have hamartomas in their digestive tract. Peutz-Jeghers syndrome is also associated with a higher than average risk of other types of cancer, including cancers of the breast, pancreas, stomach, ovary, lung and breast. the small intestine.
Hereditary mixed polyposis syndrome is an inherited condition that results in the growth of many different types of polyps. Hamartoma is the most common type of polyp that manifests itself.
Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome are in a group of conditions that have a mutation in the PTEN gene, which is usually a tumor suppressor gene. People with the PTEN mutation are more likely to develop non-cancerous and cancerous tumors, including colorectal cancer.
Physical inactivity
People who are not physically active have a higher risk of colorectal cancer.
Overweight or obese
Colorectal cancer occurs more often in people who are overweight or obese than in people who are at a healthy weight. A high body mass index (BMI) increases the risk in both men and women, although men appear to be at higher risk.
Alcohol
People who drink 45 g (about 3 drinks) of alcohol per day have a 1.5 times greater risk of colorectal cancer than non-drinkers. Alcohol increases the risk in both men and women, although the effect appears to be stronger in men.
Smoking tobacco
Smoking tobacco increases the risk of colorectal cancer. The risk seems to increase with the length of time you smoke and the amount smoked.
Diet rich in red meat
A diet rich in red meat (beef, pork, lamb and goat) increases the risk of colorectal cancer. The risk increases with the amount of red meat a person consumes.
Processed meats
Processed meats are meats that are preserved by smoking, drying, salting or adding preservatives such as nitrites or nitrates. Eating processed meats increases the risk of colorectal cancer, and this risk increases with the amount consumed.
Low fiber diet
Eating a diet low in fiber increases the risk of colorectal cancer. There is some evidence that consuming foods containing dietary fiber provides protection against colorectal cancer.
Sedentary behavior
Frequent sedentary behavior (sitting for long periods of time) has been linked to an increased risk of colorectal cancer, especially cancer of the distal colon and rectum.
Inflammatory bowel disease (IBD)
IBD affects the lining of the digestive tract, which becomes inflamed, causing damage and bleeding. Ulcerative colitis and Crohn’s disease are the 2 most common types of IBD. Ulcerative colitis increases the risk of colorectal cancer more than Crohn’s disease. The risk increases with the duration of IBD and the extent of IBD in the colon.
Diabetes
In people with type 2 diabetes, the incidence rate of colorectal cancer is higher. There is a link between the two since the risk factors for diabetes – physical inactivity and being overweight or obese – are also risk factors for colorectal cancer.
Ashkenazi Jewish descent
People of East European Jewish descent (Ashkenazi Jews) have a higher than average risk of colorectal cancer. A particular mutation in the APC gene that increases the risk of colorectal cancer tends to be present in this group of people. This genetic mutation is not common in other ethnic groups.
Personal history of breast, ovarian or uterine cancer
A woman who has had breast, ovarian or uterine cancer is at greater risk for colorectal cancer. This increased risk may be due to common risk factors, including Peutz-Jeghers syndrome, Ashkenazi Jewish descent, Lynch syndrome, or certain other genetic syndromes.
Tall adult height
Several studies show that height is a risk factor for colon cancer, but probably not for rectal cancer. Researchers believe this is due to the influence of growth hormones and puberty.
Cooking meat at high temperature
Cooking meat (including beef, pork and poultry) and fish to a high temperature (i.e. well done, fried, broiled or barbecued) forms chemicals called heterocyclic amines (HAs) . Some HAs have been linked to an increased risk of colorectal cancer.
The fat that runs off meat, poultry and fish on coals or hot stones generates other potentially carcinogenic substances called polycyclic aromatic hydrocarbons (PAHs). These, caused by smoke and flames, are added to food. Some of these PAHs are associated with an increased risk of colorectal cancer.
Exposure to ionizing radiation
People who have been exposed to ionizing radiation, for example during atomic bomb explosions in Japan, are at increased risk of developing colorectal cancer, especially colon cancer. People who have been treated with radiation therapy for a previous cancer have a greater risk of colorectal cancer.
Possible risk factors
The following factors have been linked to colorectal cancer in some way, but there is insufficient evidence to suggest that they are risk factors. More research is needed to clarify the role of these factors in the development of colorectal cancer.
Asbestos is a group of natural minerals. Asbestos has been used extensively in building materials and many industries. Asbestos is recognized as a carcinogen. Prolonged and frequent exposure to asbestos could cause colorectal cancer.
Cystic fibrosis is a genetic disorder that affects the glands that make mucus and sweat, which can affect how the lungs and digestive tract work. A large study that followed people with cystic fibrosis for 20 years showed that they may be at increased risk for colorectal cancer.
No link to colorectal cancer
Significant research shows no link between laxatives and an increased risk of colorectal cancer.
Grades of colorectal cancer
The grade, or histological classification, defines how cancerous cells look when compared to normal, healthy cells. Knowing the grade gives your healthcare team an idea of how quickly cancer can grow and how likely it is to spread. It helps him plan your treatment. The grade can also help the healthcare team determine the possible outcome of the disease (prognosis) and how the cancer might respond to treatment.
To establish the grade of colorectal cancer, the pathologist examines a sample of tissue taken from the tumor under a microscope. It checks how much cancer cells differ from normal cells (differentiation) and from other characteristics of the tumor such as the size and shape of cells and their arrangement. He can usually tell how fast the tumor is growing by looking at the number of dividing cells.
The pathologist assigns a grade of 1 to 3 or 4 to colorectal cancer. The lower this number, the lower the rank.
Low-grade cancers are made up of well-differentiated cancer cells. These cells are abnormal, but they look a lot like normal cells and are arranged very similarly to normal cells. Low-grade cancers tend to grow slowly and are less likely to spread.
High-grade cancers are made up of poorly differentiated or undifferentiated cancer cells. These cells do not look like normal cells and are arranged very differently. High grade cancers tend to grow quickly and are more likely to spread than low grade cancers.
http://cleverlysmart.com/tumor-markers-what-tests-used-to-diagnose-detect-and-monitor-cancer/
Stages of colorectal cancer
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. Information from tests is used to find out how big the tumor is, which parts of the colon or rectum have cancer, whether the cancer has spread from where it originated, and where it spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The most frequently used staging system for colorectal cancer is the TNM classification. In colorectal cancer, there are 5 stages, ie stage 0 followed by stages 1 to 4. For stages 1 to 4, the Roman numerals I, II, III and IV are often used. But in order to make the text clearer, we will use the Arabic numerals 1, 2, 3 and 4. In general, the higher the stage number, the more cancer has spread. Talk to your doctor if you have questions about staging.
When doctors describe the stage, they can use the words local, regional, or distant. Local means the cancer is only found in the colon or rectum and has not spread to other parts of the body. Regional means near or around the colon or rectum. Distant means in a part of the body farther from the colon or rectum.
If colorectal cancer spreads
Cancer cells can spread from the colon or rectum to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer usually grows and spreads helps your healthcare team plan your treatment and future care. If colorectal cancer spreads, it can spread to the following parts of the body:
- nearby lymph nodes (the place where colorectal cancer most often spreads)
- neighboring tissues in the abdomen or pelvis
- peritoneum
- distant lymph nodes
- kidneys
- adrenal glands
- liver
- lungs
- bone
- brain
http://cleverlysmart.com/tumor-markers-what-tests-used-to-diagnose-detect-and-monitor-cancer/
Treatments for colorectal cancer
If you have colorectal cancer, your healthcare team will create a treatment plan just for you. It will be based on your health and specific cancer information. When your healthcare team decides which treatments to offer you, they take the following into consideration:
- the location of the tumor or where the cancer has come back (recurred)
- the stage of cancer
- your general state of health
- what you prefer or want
You may be offered one or more of the following treatments for colorectal cancer
Surgery
Surgery is the main treatment for most colorectal cancers. Depending on the stage and location of the tumor, one of the following types of surgery may be done.
Local excision (local resection) is surgery that removes abnormal tissue, such as a polyp or tumor, along with a margin of healthy tissue around it. It is usually used to remove a stage 0 colorectal tumor, some stage 1 rectal tumors, or a local recurrence of rectal cancer. Types of local excision are polypectomy, local transanal excision, and transanal endoscopic microsurgery.
Resection of the bowel is the most common type of surgery for colorectal cancer. It involves removing part of the intestine and nearby lymph nodes. Depending on the location of the tumor, one of the following types of bowel resection is done:
- right hemicolectomy to remove the right side of the colon
- transverse colectomy to remove the central part of the colon
- left hemicolectomy to remove the left side of the colon
- sigmoid colectomy to remove the last part of the colon
- low anterior resection to remove the last part of the colon and part of the rectum
- proctocolectomy to remove the rectum and part of the sigmoid colon (last part of the colon)
- abdominoperineal resection to remove the rectum, anal canal and neighboring muscles
- partial colectomy to remove most of the colon
- total colectomy to remove the entire colon
- A colostomy or an ileostomy can be done after a bowel resection.
These surgeries can also help bypass or prevent a blockage in the intestine, known as a bowel obstruction. A stoma (artificial opening) is created in the colon or ileum to the outside of the body through the wall of the abdomen. Colostomy and ileostomy are temporary or permanent.
Lymph node dissection is surgery to remove lymph nodes near the tumor and is done during bowel resection.
A pelvic exenteration can be done to treat stage 4 or recurrent rectal cancer that has spread to nearby organs. The reproductive organs are removed as well as the lymph nodes in the pelvis. Usually part of the colon and the rectum or both are removed. Sometimes the bladder is also removed.
Surgery is done to remove metastatic tumors when there are only one or a few in the liver or lungs.
Cancer Surgery (Operation): Understanding Types, Risks, and Recovery
Chemotherapy
Chemotherapy is sometimes used to treat colorectal cancer. The following chemotherapy drugs can be used alone or in combination to treat colorectal cancer:
- 5-fluorouracil (Adrucil, 5-FU)
- capecitabine (Xeloda)
- oxaliplatin (Eloxatin)
- irinotecan (Camptosar)
- raltitrexed (Tomudex)
- trifluridine and tipiracil (Lonsurf)
- Leucovorin (folinic acid) is commonly used to treat colorectal cancer. It is not a chemotherapy drug, but it does make 5-fluorouracil more effective.
Chemotherapy Drugs Combinations | Chemo Medications: Understanding Medications for Cancer Treatment
Chemoradiotherapy
Chemotherapy is often combined with radiation therapy to treat rectal cancer. This is called chemoradiation. The 2 treatments are administered during the same period. The chemotherapy drugs that are usually used are 5-fluorouracil or capecitabine.
Radiotherapy
Radiation therapy is mostly used to treat rectal cancer. It can be given on its own or combined with chemotherapy as part of chemoradiation.
External beam radiation therapy is the most common type of radiation therapy. Brachytherapy may be used in some cases.
Targeted treatment
Targeted therapy is sometimes used to treat advanced colorectal cancer. It is usually taken with chemotherapy, but it can be given on its own.
The following targeted drugs can be used to treat colorectal cancer:
- bevacizumab (Avastin, Mvasi)
- cetuximab (Erbitux)
- panitumumab (Vectibix)
- regorafenib (Stivarga)
Targeted therapy for cancer patients | Types, Receiving treatment, Side effects
Colon cancer survival rate
If you have colorectal cancer, you may have questions about your prognosis. A prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type of cancer you have, the stage and other characteristics of the disease, the treatments chosen and the response to treatment can review all of this data together with survival statistics. to arrive at a prognosis.
A prognostic factor is an aspect of cancer or a characteristic of the person that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. We often discuss prognostic and predictive factors together. They both play a role in choosing the treatment plan and in establishing the prognosis.
The following are the prognostic or predictive factors for colorectal cancer.
Stadium
Stage is the most important prognostic factor in colorectal cancer. The lower the stage at diagnosis, the better the outcome. Tumors that are only present in the colon or rectum have a better prognosis than those that have passed through the wall of the colon or rectum or that have spread to other organs (distant metastases).
Surgical margins
When removing a colorectal tumor, the surgeon also removes a margin of healthy tissue from all around it. The prognosis is better when there are no cancer cells in the tissue removed with the tumor than when cancer cells are observed in this tissue, that is, the surgical margins are positive.
Cancer cells in the blood and lymphatic vessels
Cancer cells can travel or grow in blood vessels and lymphatic vessels near the tumor. It is lymphovascular invasion. If there is no lymphovascular involvement, the prognosis is better than if there is lymphovascular involvement.
Carcinoembryonic antigen level
Carcinoembryonic antigen (CEA) is a protein that is normally found in very small amounts in the blood of adults. There may be an increase in the blood level of CEA in the presence of certain types of cancer and non-cancerous (benign) conditions. The lower the ACE level before surgery, the better the prognosis.
Bowel obstruction or perforation
Bowel obstruction is a blockage in the intestine. Intestinal perforation is a hole or tear in the intestine. People whose intestines are blocked or perforated at diagnosis have a poorer prognosis.
Grade
High-grade colorectal cancer is made up of cancer cells that are poorly differentiated or undifferentiated. High-grade cancers have a poorer prognosis than low-grade cancers.
Tumor type
Mucinous adenocarcinoma, ring cell carcinoma and small cell carcinoma have a poorer prognosis than other types of colorectal tumors.
Microsatellite instability (MSI)
MSI is a change in the DNA of a cell. Some colorectal cancer cells have ISD. Tumors whose cells exhibit a high microsatellite instability generate a better prognosis than tumors whose microsatellites are not very unstable (microsatellite stability, or MSS). High MSI is seen in 20% of people with stage 2 colorectal cancer, in 10% of people with stage 3 colorectal cancer, and in less than 5% of people with stage colorectal cancer. 4.
Mutation of the KRAS gene
The KRAS gene can be changed (mutated) in some colorectal cancer cells. The presence of mutations in the KRAS gene means that cancer cells are unlikely to respond to targeted drugs. People whose colorectal cancer cells have the KRAS gene mutation have a poorer prognosis because the targeted drugs will not work on the tumor.
BRAF gene mutation
The presence of mutations in the BRAF gene means that cancer cells can be more aggressive. Thus, people whose colorectal cancer cells have the BRAF gene mutation have a poorer prognosis. Less than 10% of all colorectal cancers have the BRAF gene mutation.
Supportive care for colon cancer (colorectal cancer)
Supportive care empowers people to overcome the physical, practical, emotional and spiritual barriers of colorectal cancer. It is an important component of the care of people with this disease. There are many programs and services that meet the needs and improve the quality of life of these people and their loved ones, especially after treatment is over.
Recovering from colorectal cancer and adjusting to life after treatment is different for everyone, depending on the stage of the cancer, the organs and tissues removed during surgery, the type of treatment given and many other factors. The end of cancer treatment can lead to mixed emotions. Even if treatment is finished, there may be other issues to work out, such as coping with long-term side effects. A person who has been treated for colorectal cancer may be concerned about the following.
Self-esteem and body image
Self-esteem is how we feel about ourselves. Body image is how we perceive our own body. Colorectal cancer and its treatments can affect a person’s self-esteem and body image. This is often because cancer or treatments can cause changes in the body such as the following:
- scars
- skin problems
- change in body weight
- presence of a stoma following a colostomy or an ileostomy
Some of these changes may be temporary. Others can last a long time or be permanent.
Living with a colostomy or ileostomy
A colostomy is the creation of a stoma (artificial opening) in the colon to the outside of the body through the abdominal wall. An ileostomy involves creating a stoma in the ileum to the outside of the body through the abdominal wall. Colostomy and ileostomy can be temporary or permanent.
Not all people with colorectal cancer will need a colostomy or ileostomy.
It takes time and patience to learn how to live with and care for an ostomy. Specially trained nurses will teach you and your family how to live with and care for an ostomy. They are enterostomal therapists (ST), specialized in wound care, ostomy and continence. Support and information can be obtained from local or national ostomy associations or groups.
Nutrition
Maintaining an adequate diet is an important part of life after colorectal cancer, especially because cancer and its treatments affect the digestive system. Most people can eat normally after surgery and other treatments for colorectal cancer.
Some people need to change their diet because they experience the following conditions, which may affect their nutrition. Ask your healthcare team to refer you to a dietitian.
Diarrhea
Diarrhea is often a problem for people who have had a bowel resection. Diarrhea is more likely to occur if a large part of the large intestine has been removed.
Your large intestine usually absorbs water. When part of your large intestine, including the colon, is removed, it cannot absorb water normally. This causes diarrhea. Having diarrhea because part of the bowel has been removed is called short bowel syndrome.
You can help manage diarrhea by changing your diet. Limiting your intake of certain foods and drinks, such as fatty or high-fiber foods, coffee, tea, and alcohol, can help prevent diarrhea. You may be given medicine to help treat diarrhea.
Constipation
Surgery to treat colorectal cancer can change the structure and function of the bowel. The intestine can become narrow after a resection. It is also possible to damage muscles and nerves during an operation. These changes may affect the normal formation of feces (stools) and their movement in the large intestine, causing constipation.
You can help manage constipation by drinking plenty of fluids every day and being physically active. Laxatives and enemas can also help treat constipation.
Sexuality
Treatments for colorectal cancer can cause sexual problems or make sex difficult. Some people may lose interest in sex during the process of diagnosis and treatment.
Talk to your doctor or healthcare team if you have sexual problems with colorectal cancer and its treatments. They can help you manage them. Some people find that counseling helps them cope with the effects of colorectal cancer and its treatments on their sex. Sometimes taking medication helps treat sexual problems.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, American Cancer Society, Web MD, Cancer Center, Cleveland Clinic
Photo credit: Wikimedia Commons
Photo explainations: The location and appearance of two types of colorectal tumors.