What is cervical cancer?
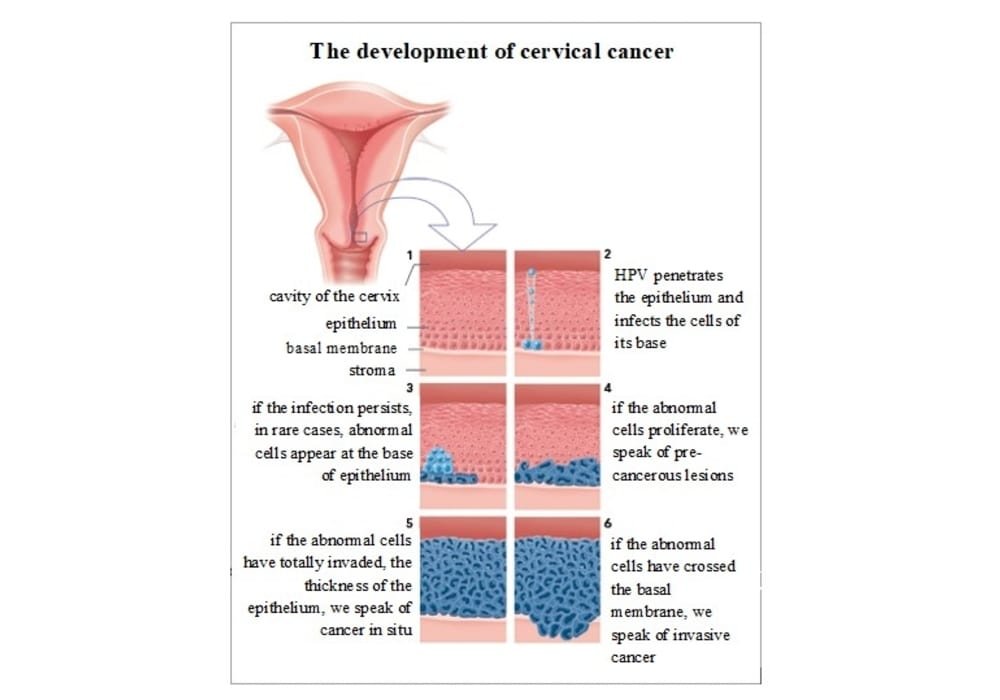
Cervical cancer starts in cells of the cervix. Cancerous (malignant) tumor is a group of cancer cells that can invade and destroy nearby tissue. The tumor can also spread (metastasize) to other parts of the body.
The cervix is part of the female reproductive system. It is the lower, narrow part of the uterus (uterus) that opens at the top of the vagina and serves as a passage connecting the uterus to the vagina.
Cells in the cervix sometimes undergo changes that make the way they grow or behave abnormally. These changes can lead to the formation of non-cancerous (benign) tumors such as polyps, cysts or fibroids.
Changes in the cells of the cervix can also cause precancerous conditions. This means that these abnormal cells are not yet cancerous, but they are likely to become cancerous if left untreated for a long time. The most common precancerous condition of the cervix has different names depending on how it is classified or how it is recorded. The most common classifications of precancerous conditions of the cervix use the terms squamous intraepithelial injury (SIL), cervical intraepithelial neoplasia (CIN), or cervical dysplasia.
In some cases, changes in cells can turn into cervical cancer. Most of the time, cervical cancer starts in flat, round cells called squamous cells. These cells line the outer part of the cervix. This type of cancer is called squamous cell carcinoma of the cervix. Cancer can also start in other cells called gland cells. These cells line the passage that connects the uterus to the vagina. This type of cancer is called adenocarcinoma of the cervix.
Rare types of cervical cancer can also occur. Examples are adenosquamous carcinoma, vitreous cell carcinoma and mucoepidermoid carcinoma.
The cervix
The cervix is part of the female reproductive system. This device is made up of internal organs, including the vagina, uterus, ovaries and fallopian tubes. It is also made up of the external genitalia, including the parts that make up the vulva (clitoris, labia and orifice of the vagina). All of the internal organs are located in the pelvis, which is the lower part of the abdomen between the hip bones.
The cervix is the lower, narrow part of the uterus (uterus). It connects the main body of the uterus to the vagina (birth canal).
Function of the cervix
The cervix connects the body of the uterus to the vagina. Part of the lining of the cervix contains glands that make and release mucus. During most of the menstrual cycle and during pregnancy, this mucus is thick and does not allow semen to enter the uterus. This thick mucus also helps protect a woman’s uterus and upper reproductive organs from harmful bacteria.
When a mature egg is released from an ovary each month (ovulation), the mucus changes and becomes thinner, allowing sperm to pass through the cervix to the uterus.
Every month, except during pregnancy or menopause, the lining of the uterus (endometrium) is released from the body through the cervix and then the vagina. This process is called menstruation.
During childbirth, the cervix widens, or dilates, to allow the baby to pass through the birth canal.
In short!
Cervical cancer is a type of cancer that develops in the cells of the cervix, which is the lower part of the uterus that connects to the vagina. It is one of the most common types of cancer affecting women worldwide.
Causes
The primary cause of cervical cancer is infection with certain types of the human papillomavirus (HPV), which is a common sexually transmitted infection. Other risk factors for cervical cancer include smoking, a weakened immune system, a family history of cervical cancer, and early sexual activity.
Symptoms
Early cervical cancer may not produce any noticeable symptoms, which is why regular Pap smears and HPV tests are important for early detection. As the cancer grows, symptoms may include abnormal vaginal bleeding, pain during sexual intercourse, and pelvic pain.
Diagnosis
Cervical cancer is typically diagnosed through a Pap smear or an HPV test, which can detect abnormal cells or the presence of the virus. If abnormal cells are detected, further testing may be done, including a colposcopy (a procedure to examine the cervix) and a biopsy (a sample of tissue taken from the cervix).
Treatment
Treatment for cervical cancer depends on the stage of the cancer and may include surgery, radiation therapy, chemotherapy, or a combination of these. Early-stage cervical cancer may be treated with surgery or radiation therapy, while more advanced cases may require a combination of treatments.
Prevention
Cervical cancer can be prevented through the HPV vaccine, which is recommended for both boys and girls before they become sexually active. Regular Pap smears and HPV tests are also important for early detection and treatment. Other prevention measures include practicing safe sex, not smoking, and maintaining a healthy immune system.
Cancerous tumors of the cervix
Cancerous tumor of the cervix can invade and destroy nearby tissue. It can also spread (metastasize) to other parts of the body. Cancerous tumor is also called a malignant tumor.
Squamous cell carcinoma and adenocarcinoma are the most common tumors of the cervix. These types of cervical cancer usually develop from precancerous changes inside the cervix that are caused by infection with the human papillomavirus (HPV). Most precancerous changes in the cervix do not develop into cancer. When they do, it usually takes several years.
Squamous cell carcinoma
Most cervical cancers are squamous cell carcinomas. This type of cancer starts in the squamous cells that line the outer surface of the cervix, the ecocervix. Squamous cell carcinoma most often appears in the squamocolumnar junction. This region is also called the transformation zone since column cells are constantly changing into squamous cells, which is part of a normal process.
Squamous cell carcinoma can be keratinizing or non-keratinizing.
Keratinizing means squamous cells develop into masses (nests) of cells that contain keratin (a resistant fibrous protein).
Non-keratinizing means squamous cells develop into nests of cells that do not contain keratin.
Rare types of squamous cell carcinoma of the cervix include verrucous carcinoma, papillary carcinoma, transitional papillary carcinoma, condylomatous carcinoma, basaloid carcinoma and lymphoepithelial carcinoma.
Adenocarcinoma
Most other cervical cancers are adenocarcinomas. Adenocarcinoma starts in the glandular cells that line the inside of the cervix, called the endocervix.
Mucinous adenocarcinoma is the most common type of cervical adenocarcinoma.
Endometrioid adenocarcinoma is a type of cancer-like adenocarcinoma that appears in the lining of the uterus.
Clear cell carcinoma can occur in the daughters of women who took diethylstilbestrol (DES) during pregnancy.
Rare types of cervical adenocarcinoma include serous papillary adenocarcinoma, villoglandular papillary adenocarcinoma, mesonephroid adenocarcinoma, and endocervical microcystic adenocarcinoma.
Adenosquamous carcinoma
Adenosquamous carcinoma is made up of a mixture of glandular cells and squamous cells. It can affect women of any age.
Vitreous cell carcinoma is an aggressive form of adenosquamous carcinoma.
Rare tumors of the cervix
The following cancerous tumors of the cervix are rare:
- small cell carcinoma
- mucoepidermoid carcinoma
- adenoid cystic carcinoma
- malignant Müllerian mixed tumor
- basal adenoid carcinoma
- primary neuroectodermal tumor
- small round cell desmoplastic tumor
- carcinoid tumor
- primary germ cell tumor
- neuroendocrine carcinoma
- primary extranodal lymphoma
- sarcoma
- melanoma
Precancerous conditions of the cervix
Precancerous conditions of the cervix are changes in the cells of the cervix that make them more likely to become cancerous. These conditions are not yet cancerous, but the abnormal changes in cells could turn into cervical cancer if left untreated. An untreated precancerous cervical condition can take up to 10 years or more to develop into cervical cancer, but in rare cases it happens in less time.
Precancerous conditions of the cervix start in an area called the transformation zone. This is where columnar cells (a type of glandular cell) constantly change into squamous cells. The transformation of columnar cells into squamous cells is a normal process, but it makes cells more susceptible to the effects of human papillomavirus (HPV).
Types of precancerous conditions
Precancerous conditions of the cervix are described based on the degree of abnormality in the appearance of cells seen under a microscope and the severity of the cellular changes. They are grouped according to the type of cell that is abnormal. Precancerous changes in the cervix are quite common.
Abnormal squamous cells
Most doctors use the Bethesda system to describe abnormal changes to squamous cells in the cervix where they are called squamous intraepithelial lesions (SIL). Other systems use the terms cervical intraepithelial neoplasia (CIN) or cervical dysplasia instead.
SILs are low grade or high grade. The CINs are grade 1, 2 or 3.
Low-grade SIL (LSIL) is comparable to CIN 1. LSIL only affects cells that are on or near the surface of the lining of the cervix. Cervical dysplasia is mild, and the cells have undergone changes that make them only slightly different from normal cells.
High-grade SILs (HSILs) are comparable to CINs 2 and 3. The changes in cells are deeper in the lining of the cervix. Cervical dysplasia is moderate or severe and the cells are considered more abnormal.
In the case of HSILs, cells show marked changes in size and shape, so they look different from normal cells. CIN 2 is moderate to severe dysplasia. CIN 3 is severe dysplasia and also includes carcinoma in situ. The higher the grade, the greater the risk of cancer.
Abnormal glandular cells
Atypical glandular cells (AGC) and adenocarcinoma in situ (AIS) are characterized by changes in glandular cells in the cervix. Glandular cell abnormalities are not graded but are described using the Bethesda System.
AGC means the cells don’t look normal. Changes to these cells increase the risk of developing into cancer or may mean that there is an underlying cancer.
AIS means that preinvasive cancer cells have been seen, that is, they have not spread to the deeper tissues of the cervix or to nearby tissues.
Risk factors
Human papillomavirus (HPV) infection is the main risk factor for precancerous changes in the cervix. Smoking and a weakened immune system increase the likelihood that an HPV infection will not go away on its own and develop into a precancerous condition of the cervix.
Symptoms
Precancerous changes in the cervix usually do not cause any signs or symptoms. The abnormal Pap test result is often the first sign that certain cells in the cervix are abnormal. This is why it is important to have a regular Pap test.
Diagnostic
If the result of a Pap test is abnormal, you will have further tests to rule out or diagnose a precancerous condition or cervical cancer. Reviews may include these:
- another Pap test a few months later (usually 6 months) if the changes are slight
- an HPV test, which is sometimes done on a sample of cervical cells taken during a Pap test
- a colposcopy and biopsy of any area that appears abnormal
- endocervical curettage, to remove cells from the endocervical canal usually during colposcopy
Treatments
Most women treated for precancerous cervical condition have an excellent prognosis and this condition will never develop into cervical cancer.
Mild cervical abnormalities often go away on their own and return to a normal life without treatment.
More severe abnormalities are more likely to progress to cervical cancer, especially if left untreated for a long time. It is difficult to predict which ones will develop into invasive cervical cancer, so treatment is usually started as soon as they are diagnosed.
Treatment options for precancerous changes in the cervix may include the following:
- loop electrosurgical excision technique (LEEP) or other type of conical biopsy
- cryosurgery
- laser surgery
- hysterectomy
Non-cancerous tumors of the cervix
A non-cancerous (benign) tumor of the cervix is a lump that does not spread to other parts of the body (not metastasize). The non-cancerous tumor is usually not life threatening. It is usually removed by surgery and usually does not come back (come back).
Cervical polyp
The cervical polyp is the most common non-cancerous tumor of the cervix. Most polyps are non-cancerous, but some can be cancerous (malignant).
The cervical polyp most often appears in women over the age of 20. It is rare in young women who have not yet menstruated. It is a red mass similar to a finger. It starts in the endocervical canal (the passage that connects the uterus to the vagina) and can advance into the vagina.
The cervical polyp may not be causing symptoms. Some women may have abnormal vaginal bleeding or a vaginal discharge varying from yellow to white. The cervical polyp can be detected when the doctor does a pelvic exam and a Pap test.
You don’t usually need to treat a cervical polyp. If it’s big, bleeding, or looks abnormal, it can be removed, usually with a pelvic exam.
Naboth’s cyst
Naboth’s cyst is a mucus-filled lump that appears on the surface of the cervix. Most women have Naboth cysts and their presence is normal. They are usually detected during a routine pelvic exam and appear as a small, smooth, rounded mass or as a lump on the cervix.
Naboth’s cyst usually does not require treatment. In some cases, it can grow large enough to change the shape of the cervical canal and make pelvic exams difficult. At this point, the cyst can be opened to remove the mucus (drainage) or it can be removed.
Cervical fibroma
Cervical fibroids (myoma) start in muscle tissue in the cervix. It looks like uterine fibroid, but it is less common.
It is possible that the cervical fibroid is not causing symptoms. Abnormal vaginal bleeding is the most common symptom. Pain can be present during sex. If the fibroid becomes large, it may partially block the urinary tract and cause problems with passing urine such as leakage or retention. Urinary tract infections can also appear.
Cervical fibroids usually do not need to be treated unless they are causing symptoms. Treatment includes taking medication to control symptoms or having surgery to remove the fibroid.
Risk factors for cervical cancer
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors. The most important risk factor for cervical cancer is human papillomavirus (HPV) infection, but it does not always cause the disease on its own. We now know that other risk factors (cofactors) work together with HPV to increase the risk of cervical cancer.
The majority of cervical cancers appear in women under the age of 50. Cervical cancer tends to affect women of African descent more than whites. Rates of cervical cancer also tend to be lower in women belonging to certain religious communities, such as Catholic nuns and Amish or Mormon women. This is probably because of the small number of sexual partners these women have, which could reduce their exposure to HPV.
Women with low incomes and those with less education are at greater risk of developing cervical cancer. This may be because these women do not get tested regularly or because they have other risk factors, such as higher smoking rates.
Precancerous conditions of the cervix include squamous intraepithelial lesions (SIL). It’s not cancer, but sometimes they can turn into cervical cancer if left untreated. Some of the risk factors for cervical cancer can also cause these precancerous conditions.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
Risk factors
There is convincing evidence that the following factors increase your risk for cervical cancer.
- Human papillomavirus (HPV) infection
- Sexual activity
- Smoking
- Multiple deliveries
- Human immunodeficiency virus (HIV) infection
- History of sexually transmitted infections (STIs)
- Oral contraceptives
- Diethylstilbestrol (DES)
Human papillomavirus (HPV) infection
The majority of women who have cervical cancer have had an HPV infection in the past. But having an HPV infection doesn’t mean you will have cervical cancer. Many different types of HPV can infect the cervix, but only a few cause abnormal changes in cells that can develop into cancer.
Sexual activity
Being sexually active means more than just having sex with someone. It could be:
- any genital skin (skin to skin) contact;
- oral sex.
All women who have ever been sexually active are at risk of developing cervical cancer because sexual activity can expose them to HPV. This type of cancer rarely appears in women who have never been sexually active.
Becoming sexually active at a young age can increase your risk of developing cervical cancer. Researchers believe that this increased risk is attributable to changes that occur in the cervix during puberty that make this area more vulnerable to injury.
Certain types of sexual behavior increase a woman’s risk of HPV infection. Having sex with many partners can increase exposure to HPV, which is transmitted sexually. This is why many sexual partners have been linked to an increased risk of cervical cancer. However, a woman can be infected with HPV even if she has only had one sexual partner.
Women also appear to be at greater risk of developing cervical cancer if their male partners have had multiple sexual partners or female partners with cervical cancer.
Smoking
Smoking makes an HPV infection more likely to not go away on its own. If an HPV infection does not go away, it can lead to the formation of a squamous intraepithelial lesion (SIL), which is a precancerous condition of the cervix, as well as the development of cervical cancer uterus.
Multiple deliveries
Parity is the number of times a woman has given birth to a child, or given birth. Multiparity, meaning giving birth more than once, has been linked to the risk of cervical cancer uterus in women with HPV infection. This risk increases with the number of times a woman gives birth. But the risk does not increase with a specific number of deliveries.
It is not yet fully understood how childbirth increases the risk of cervical cancer. This may be because of hormonal changes that occur during pregnancy or the trauma to the cervix during childbirth. Some research suggests that women who have cesarean sections are not at an increased risk for cervical cancer.
Human immunodeficiency virus (HIV) infection
The human immunodeficiency virus (HIV) weakens the immune system. A weakened immune system increases your risk of getting other infections, including HPV. Having a weaker immune system also increases the risk that an HPV infection will not go away. HIV increases the risk that precancerous changes in the cells of the cervix will develop into cervical cancer.
Women who are HIV-positive are at higher risk of developing cervical cancer, and precancerous cells turn into cancer more quickly in HIV-positive women than in HIV-negative women.
History of sexually transmitted infections (STIs)
Chlamydia trachomatis is a type of bacteria. It is spread through sexual contact and can infect the female genital tract. Women with HPV and chlamydia infections have a higher risk of developing cervical cancer. Researchers believe that prolonged inflammation caused by chlamydia makes it harder for the body to get rid of the HPV infection, especially if chlamydia infections follow one another.
Herpes simplex virus type 2 is also called human herpesvirus 2 or HHV-2. HHV-2 infection can also be linked to an increased risk of cervical cancer in women with HPV.
Oral contraceptives
Oral contraceptives are commonly called the pill. Long-term use of oral contraceptives may increase the risk of HPV infection developing into cervical cancer. This risk does not appear to be related to the presence of an HPV infection. Women who take oral contraceptives for more than 5 years seem to be the most likely to get cervical cancer. However, this risk decreases over time after you stop taking birth control pills. Ten years after you stop taking birth control pills, your risk of cervical cancer is no longer.
Diethylstilbestrol (DES)
Diethylstilbestrol (DES) is a form of estrogen that was used between 1940 and 1971 to treat women with certain problems during pregnancy, such as miscarriages. It has not been approved for use in pregnant women since 1970.
Girls of women who took DES during their pregnancy have a higher than average risk of developing a rare type of cervical cancer called clear cell carcinoma. Some studies also suggest that the daughters of women who have taken DES may be at higher risk for precancerous changes in the cervix and squamous cell carcinoma of the cervix.
Possible risk factors
Taking immunosuppressants is a possible risk factor for cervical cancer. This means that immunosuppressants have been linked to cervical cancer, but there is not enough evidence to say that this is a risk factor.
There is some evidence that these drugs may increase the risk of cervical cancer in women who have had an organ transplant. Results in women taking immunosuppressants for an immune disorder such as systemic lupus erythematosus or inflammatory bowel disease (ulcerative colitis or Crohn’s disease) are inconclusive.
Reduce the risk of cervical cancer
You can reduce your risk of cervical cancer by doing the following things.
Get vaccinated against the human papillomavirus (HPV)
HPV is a risk factor for squamous intraepithelial lesions (SIL), which is a precancerous condition, and cervical cancer. The 3 HPV vaccines available in Canada are Gardasil, Cervarix and Gardasil 9. These vaccines help protect against infection with HPV 16 and HPV 18, the 2 types of HPV most commonly associated with precancerous conditions and cancer of the breast. cervix. The Gardasil 9 vaccine also protects against 5 other types of HPV that can cause cancer. These 3 vaccines are approved to help prevent precancerous conditions of the cervix and cervical cancer associated with HPV infection.
Get vaccinated or have your children vaccinated through school programs if available. If you are not eligible for the free vaccination, ask your doctor which vaccine you should get and when.
HPV vaccines should be an adjunct, not a substitute for cervical cancer screening. All women, whether or not they get the HPV vaccine, should be tested for cervical cancer. HPV vaccines prevent infection from the types of HPV associated with 70-90% of all cervical cancers. So not all HPV vaccines prevent cervical cancer.
Adopt safer sex practices
The safest way to prevent HPV infections is to avoid genital contact with another person. A person who has had sex before is at risk of getting HPV.
Ask your partners if they have or have ever had a sexually transmitted infection (STI) and if they always protected themselves. Remember that your partners’ previous sexual behaviors are also a risk factor for you, especially if they have had multiple partners.
If you have an active sex life, use condoms or other barriers, such as dental dams, to help protect yourself from HPV. Using condoms or other barriers can reduce the risk of HPV infection if they are put on before skin-to-skin sexual contact. However, uncovered skin is not protected against the virus.
Follow cancer screening guidelines
If you follow the guidelines for screening for cervical cancer, the cancer can be detected before you see symptoms. Follow the guidelines even when you are feeling good and healthy. Have a regular Pap test to help find abnormal changes in your cervix as soon as possible.
Screening is checking to see if the disease is present in a group of people who do not have symptoms of the disease. Screening tests can find cervical cancer before any symptoms appear. When cervical cancer is detected and treated at an early stage, the chances of successful treatment are better.
If you’ve been sexually active before, you should start having a regular Pap test from age 21. The Pap test should be done every 1 to 3 years depending on the results of your previous exams.
Live smoke-free
Smoking tobacco increases the risk of precancerous conditions and cervical cancer. For contact information for the Smokers ‘Helpline in your province or territory, visit cancer.ca/Smokers’ Helpline.
Find out if your risk of cervical cancer is high
Some women are more likely than average to one day develop cervical cancer. Talk to your doctor about your risk. If it is above average, you may need to have a Pap test more often or an HPV test.
Symptoms of cervical cancer
Cervical cancer may not cause any signs or symptoms in the very early stages of the disease. Symptoms often appear after the tumor has grown into nearby tissues and organs. Other medical conditions can cause the same symptoms as cervical cancer.
Signs and symptoms of cervical cancer include the following:
- abnormal vaginal bleeding, including between periods, after menopause, and after sex
- abnormal or heavier vaginal discharge
- smelly vaginal discharge
- unusually long or heavy periods
- bleeding after a pelvic exam or douching
- pain during sex
- difficulty urinating
- difficulty in having a bowel movement
- leakage of urine or stools through the vagina
- pain in the pelvic area or lower back, which may extend down one or both legs
- swelling of the legs, often only one leg
- loss of appetite
- weightloss
- shortness of breath
- bloody sputum
- chest or bone pain
- tired
Diagnosis of cervical cancer
Usually, the diagnostic process for cervical cancer begins when a Pap test result is abnormal. Your doctor will ask you about your symptoms and may do a physical exam. Based on this information, your doctor will refer you to a specialist or order tests to check for cervical cancer or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay to worry, but try to remember that other medical conditions can cause symptoms similar to cervical cancer. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of cervical cancer.
The following tests are usually used to rule out or diagnose cervical cancer. Many tests that can diagnose cancer are also used to determine the stage, that is, how far the disease has spread. Your doctor may also give you other tests to check your general health and help plan your treatment.
Health history and physical examination
Your health history consists of a checkup of your symptoms, your risks, and any medical events and conditions you may have had in the past. Your doctor will ask you questions about your history:
- symptoms that suggest cervical cancer
- sexual activity
- abnormal Pap tests and treatments
- smoking
The physical exam allows your doctor to look for any signs of cervical cancer. During the physical exam, your doctor may:
- do a Pap test and pelvic exam;
- do a digital rectal exam (DRE) to look for abnormal changes;
- feel the lymph nodes in the groin and above the collarbone to see if they are swollen.
Pap test
A Pap test takes a small sample of cells from the surface of the cervix. The doctor looks at the cells under a microscope to see if they are normal or abnormal. The test finds abnormal changes in cells early, before cancer develops.
The Pap test is used to screen for cervical cancer. A Pap test is done every 1 to 3 years according to the screening guidelines in your province or territory and your health history.
HPV test
The human papillomavirus (HPV) test is a lab test that only looks for high-risk types of HPV that have been linked to cervical cancer. In some cases, this analysis can be done from the cell sample taken during the Pap test.
Colposcopy
In colposcopy, a colposcope (an instrument with a magnifying glass and light) is used to examine the vulva, vagina and cervix.
A colposcopy is done after an abnormal Pap test or positive HPV test suggests a precancerous condition or cervical cancer. A colposcopy may also be done if you have symptoms of cervical cancer.
Colposcopy is done much the same way as a Pap test. The doctor inserts a speculum into the vagina. The speculum is an instrument made of plastic or metal that separates the walls of the vagina so that the doctor can clearly see the cervix. He may apply a solution to the area that helps him see the coating on the cervix better. The doctor then uses the colposcope to carefully examine the inner surface of the cervix and vagina. He positions the colposcope outside the opening of the vagina rather than inside the vagina. The doctor may take a biopsy during the colposcopy if they see an abnormal area in the cervix.
It is best to do the colposcopy when you are not having your period. Sexual intercourse, douching and vaginal medication, as well as contraceptive creams, foams or gels (spermicides) (unless your doctor has recommended it) should be avoided 48 hours before the test as they could affect the patient. intervention and affect the results.
A pregnant woman can be colposcopy if her doctor recommends it.
Biopsy
If the result of a Pap test is abnormal, your doctor will likely do a biopsy of your cervix. During the biopsy, the doctor takes tissue or cells that he looks at under a microscope to see if cancer cells are present in the sample.
The following types of biopsy to remove cells and tissues from the cervix or nearby areas.
A colposcopic biopsy is done during a colposcopy. An anesthetic (numbing product) may be applied topically to numb the cervix. The doctor uses biopsy forceps to remove some tissue from areas of the cervix or vagina that look questionable.
Endocervical curettage is done during a colposcopy. A topical anesthetic may be applied to numb the cervix. The doctor uses a curette to gently scrape the endocervical canal to remove cells and tissue. The curette is a narrow, spoon-shaped instrument.
In an endometrial biopsy, a special instrument called a pipelle is used to remove cells from the lining of the uterus, called the endometrium, to examine them under a microscope for cancer. It can be done during the colposcopy.
A conical biopsy removes a cone-shaped piece of tissue from the cervix. The cone is formed by removing the outer part of the cervix closest to the vagina and part of the endocervical canal.
Depending on the method used, the conical biopsy can be done during the colposcopy or again in the operating room. A conical biopsy may be the only treatment needed for a precancerous condition of the cervix.
A sentinel node biopsy (BGS) removes the sentinel node to see if it is cancerous. The sentinel node is the first lymph node in a lymph node chain or cluster that receives lymph from the area around the tumor. If cancer cells spread, they are most likely to spread to these nodes first. There may be more than one sentinel node depending on the drainage route of the lymph vessels surrounding the tumor.
Complete blood count
The complete blood count (CBC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. A BSC is done to check for anemia caused by long-lasting (chronic) vaginal bleeding. The CBC also allows doctors to obtain benchmarks against which they can compare the results of future blood tests performed during and after treatment.
Blood biochemical analyzes
A blood chemistry test measures the level of chemicals in the blood. It makes it possible to evaluate the quality of functioning of certain organs and also to detect anomalies.
Blood chemistry tests are used to find out how well the kidneys and liver are functioning in the diagnostic process for cervical cancer. They also help determine whether these organs are healthy enough to tolerate and recover from the effects of cancer treatments.
Endoscopy
Endoscopy allows the doctor to observe the interior of body cavities using a flexible tube with a lumen and a lens at one end (endoscope).
During a cystoscopy, an endoscope, called a cystoscope, is used to examine the bladder and urethra. It can tell if the cancer has spread to these organs. The doctor may do a biopsy at the same time as a cystoscopy if he finds a questionable area during the exam.
During a sigmoidoscopy, an endoscope, called a sigmoidoscope, is used to examine the sigmoid colon (the last part of the colon) and the rectum. It can tell if the cancer has spread to the rectum. The doctor may do a biopsy at the same time as a sigmoidoscopy if he finds a questionable area during the exam.
Pulmonary radiography
In an x-ray, low-dose radiation is used to produce images of parts of the body on film. A chest x-ray is done to see if the cancer has spread to the lungs.
Barium enema
A barium enema is an x-ray that uses a special dye (contrast agent) called barium sulfate. A barium enema is done to see if the cancer has spread to the colon or rectum.
CT scan
A computed tomography (CT) scan uses special x-ray machines to produce 3-dimensional and cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the images in detailed pictures.
CT allows you to:
- explore the pelvis, abdomen and lymph nodes around the cervix;
- find out if the cancer has spread to other organs or tissues;
- guide the needle when biopsying an area with suspected metastasis.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) uses powerful magnetic forces and radio waves to produce cross-sectional images of the body’s organs, tissues, bones, and blood vessels. A computer assembles the images into 3-dimensional snapshots.
MRI allows you to:
- explore the pelvis, abdomen and lymph nodes around the cervix;
- find out if the cancer has spread to other organs or tissues;
- guide the needle when biopsying an area with suspected metastasis.
Intravenous urography
Intravenous urography (IVU) is a special x-ray of the urinary tract. It can be used to find out if the cancer is blocking the ureters (tubes that connect the kidneys to the bladder). IVU may not be necessary if you have had a CT or MRI.
Positron emission tomography
A positron emission tomography (PET) scan uses a radioactive material called a radiopharmaceutical to detect changes in the metabolic activity of body tissues. A computer analyzes patterns of radioactivity distribution and produces 3-dimensional, color images of the region under examination. It can be combined with CT, which is called PET / CT.
A PET can be used to find cervical cancer that has come back or has spread to other organs or tissues.
Histological classification of cervical cancer (grading)
The histological classification defines the appearance of cancer cells compared to that of normal, healthy cells. Knowing the grade gives your healthcare team an idea of how quickly cancer can grow and how likely it is to spread.
To determine the grade of cervical cancer, the pathologist examines a sample of tissue taken from the cervix under a microscope. It checks how much cancer cells differ from normal cells (differentiation) and from other characteristics of the tumor such as the size and shape of cells and their arrangement. He can usually tell how fast the tumor is growing by looking at the number of dividing cells.
The pathologist assigns a grade of 1 to 3 to cervical cancer. The lower this number, the lower the rank.
Low-grade cancers are made up of well-differentiated cancer cells. These cells are abnormal, but they look a lot like normal cells and are arranged very similarly to normal cells. Low-grade cancers tend to grow slowly and are less likely to spread.
High-grade cancers are made up of poorly differentiated or undifferentiated cancer cells. These cells do not look like normal cells and are arranged very differently. High grade cancers tend to grow quickly and are more likely to spread than low grade cancers.
Stages of cervical cancer
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. Information from tests is used to find out how big the tumor is, what parts of the organ have cancer, if the cancer has spread from where it started and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The most frequently used staging system for cervical cancer is the FIGO classification. In cervical cancer there are 4 stages. For stages 1 to 4, the Roman numerals I, II, III and IV are often used. In general, the higher the stage number, the more cancer has spread. Talk to your doctor if you have questions about staging.
Stage 0 is not included in the FIGO classification. At stage 0, we speak of a precancerous condition of the cervix or carcinoma in situ.
When doctors describe the stage, they can use the words local, regional, or distant. Local means the cancer is only found in the cervix and has not spread to other parts of the body. Regional means near or around the cervix, such as in the vagina or pelvis. Distant means in a part of the body farther from the cervix and outside the pelvis.
Some doctors may also use the following terms when talking about cervical cancer:
early stage, which usually includes stages 1A, 1B, and 2A
locally advanced, which usually includes stages 2B, 3 and 4A
advanced stage, which is usually stage 4B
Find out more about cancer staging:
Stage 1A
The tumor is in the cervix and can only be seen under a microscope. The tumor is no more than 5mm deep and no more than 7mm wide.
Stage 1A1 – The tumor is no more than 3 mm in depth and no more than 7 mm in width.
Stage 1A2 – The tumor is more than 3 mm but not more than 5 mm in depth and not more than 7 mm in width.
Stage 1B
The tumor is in the cervix and can be seen without a microscope or the tumor can only be seen under a microscope but is larger than a stage 1A tumor.
Stage 1B1 – The tumor is less than 4 cm at its widest part.
Stage 1B2 – The tumor measures over 4cm at its widest point.
Stage 2A
The tumor has grown outside the cervix and uterus but has not grown into the walls of the pelvis or the lower part of the vagina. It also did not invade the tissues just near the cervix and uterus (parameter).
Stage 2A1 – The tumor is less than 4 cm in its widest part.
Stage 2A2 – The tumor measures over 4cm at its widest point.
Stage 2B
The tumor has grown outside the cervix and uterus into the tissues near the cervix and uterus. The tumor did not grow on the walls of the pelvis or the lower part of the vagina.
Stage 3A
The tumor has grown into the lower part of the vagina but not the walls of the pelvis.
Stage 3B
The tumor has grown into the walls of the pelvis where it blocks a ureter (the channel through which urine flows from the kidney to the bladder) causing the kidney to swell (hydronephrosis) or it prevents the kidney from functioning.
OR
The cancer has spread to the lymph nodes in the pelvis.
Stage 4A
The tumor has grown in the bladder, rectum or outside the pelvis.
Stage 4B
The cancer has spread to other parts of the body (distant metastasis), such as lymph nodes outside the pelvis or the lungs, liver or bones. It is also called metastatic cervical cancer.
Recurrence of cervical cancer
Recurrence of cervical cancer means that the cancer comes back after treatment. If it reappears where it first started, it is called a local recurrence. If it reappears in tissues or lymph nodes near where it first started, it is called a regional recurrence. It can also reappear in another part of the body: this is called a recurrence or distant metastasis.
If cervical cancer spreads
Cancer cells can spread from the cervix to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer usually grows and spreads helps your healthcare team plan your treatment and future care. If cervical cancer spreads, it can spread to the following parts of the body:
- vagina
- uterus
- lymph nodes in the pelvis and back of the abdomen that are nearby
- tissues and ligaments surrounding the cervix and uterusbladder
- rectum
- lymph nodes in the chest and above the collarbones that are far apart
- abdominal cavity
- mediastinum
- lungs
- liver
- bone
Prognosis and survival for cervical cancer
If you have cervical cancer, you may be wondering about your prognosis. A prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type of cancer you have, the stage and other characteristics of the disease, the treatments chosen and the response to treatment can review all of this data together with survival statistics. to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person, such as their age or whether they smoke, that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. We often discuss prognostic and predictive factors together. They both play a role in choosing the treatment plan and establishing the prognosis.
The following are the prognostic or predictive factors for cervical cancer.
Tumor size, tumor volume and local extent
The size of the tumor is its widest part. Tumor volume corresponds to the 3 dimensions of the tumor, that is, its height, width and thickness. Small size and small volume is a better prognostic factor than large size and large volume.
Local extent refers to the depth at which the tumor has invaded the layer of connective tissue that supports the cervix as well as the tissues surrounding the cervix. The deeper the tumor has grown in these tissues, the poorer the prognosis.
Spread to the lymph nodes
One of the most important prognostic factors is the spread of cancer to the lymph nodes. Cervical cancer that has not spread to the lymph nodes has a better prognosis than cervical cancer that has spread to the lymph nodes.
Stadium (stages)
The stage of cervical cancer is an important prognostic factor. Early cervical cancer has a better prognosis than cervical cancer which is at a more advanced stage. A tumor that has grown into the sides of the pelvis, the connective tissue that surrounds the cervix and uterus or other areas of the body has a poorer prognosis than cancer that is found only in the cervix.
Lymphovascular invasion
Lymphovascular involvement means cancer is seen in the blood or lymph vessels of the tumor. Lymphatic vessels are the tubes in which lymph circulates in the body. Cancer that has not spread to the blood or lymph vessels has a better prognosis than cancer that has spread to the blood or lymph vessels.
Age and general health
Young women tend to have a better prognosis than older women. Women with good general health other than cancer also tend to have a better prognosis.
Anemia
Women with anemia seem to have a poorer prognosis than women who do not. Women with anemia also do not respond as well to radiation therapy. It is not understood why anemia has this effect in women with cervical cancer. Blood transfusion is usually not effective in reversing this effect.
Smoking
Women who smoke tend to have a poorer prognosis than women who do not smoke.
HIV status
Women who carry the human immunodeficiency virus (HIV) tend to have aggressive cervical cancer and have a poor prognosis.
Grade
Unlike most cancers, it is not known whether grade plays a role in determining the prognosis for cervical cancer in women. Some studies have shown that higher grades lead to poorer prognoses, but other studies have not found this connection.
Treatments for cervical cancer
If you have cervical cancer, your healthcare team will make a treatment plan just for you. It will be based on your health and specific cancer information. When your healthcare team decides which treatments to offer you, they take the following into consideration:
- the stage of cancer
- your age
- your general state of health
- your desire to get pregnant one day
- what you prefer or want
You may be offered one or more of the following treatments for cervical cancer:
Surgery
Depending on the stage and size of the tumor, one of the following types of surgery may be done.
A conical biopsy removes a cone-shaped piece of tissue from the cervix that includes the abnormal area. It is used to diagnose and treat early stages of cervical cancer.
An enlarged trachelectomy removes the cervix, the upper part of the vagina, certain structures and tissues surrounding the cervix (parameter) and the lymph nodes in the pelvis. It may be an option for young women with early-onset cervical cancer who want to get pregnant after treatment.
A total hysterectomy removes the cervix and uterus. It may be used to treat women with stage 1A1 cervical cancer.
A radical hysterectomy removes the cervix, uterus, parameter, and nearby lymph nodes. It may be used to treat stage 1B or stage 2 cervical cancer or cancer that comes back (comes back).
A lymph node dissection removes the lymph nodes in the pelvis to see if they contain cancer cells. Lymph node dissection is often done during surgery to help assess the outcome (establish the prognosis) and decide if further treatment is needed after the operation.
A pelvic exenteration removes the cervix, uterus, vagina, ovaries, fallopian tubes, and lymph nodes. You can also remove the rectum or the bladder or both. Sometimes a pelvic exenteration is done when cervical cancer comes back in the pelvis after being treated with radiation therapy.
In ovarian transposition, the ovaries are moved higher in the abdomen, away from the pelvis. Moving the ovaries helps protect them from possible damage from radiation therapy.
Radiotherapy
Radiation therapy can be used to treat any stage of cervical cancer. External beam radiation therapy, brachytherapy (a type of internal radiation therapy), or both can be given.
Chemoradiotherapy
Chemoradiation is the administration of chemotherapy and radiation therapy at the same time. It is used to make radiation therapy more effective. Chemoradiation therapy is commonly given to treat any stage of cervical cancer.
Chemotherapy
Only chemotherapy can be given to treat certain stages of cervical cancer.
Find out more about chemotherapy.
Targeted treatment
Bevacizumab (Avastin) is a targeted drug that can be used to treat cervical cancer that is advanced or has come back. It is usually combined with chemotherapy.
If you cannot or do not want to be treated for cancer
You may want to consider care that aims to make you feel better without treating the cancer itself, perhaps because cancer treatments no longer work, or they are no longer likely to improve your condition, or cause them to work. secondary are difficult to tolerate. There may be other reasons why you cannot or do not want to be treated for cancer.
Talk to members of your healthcare team. They can help you choose advanced cancer care and treatment.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits, especially during the first 5 years after treatment. These visits allow the healthcare team to monitor your progress and know how you are recovering from treatment.
Clinical tests
Talk to your doctor about clinical trials for cervical cancer that are underway in certain countries and are accepting participants. Clinical trials aim to find new methods of preventing, detecting and treating cancer.
Supportive care for cervical cancer
Supportive care empowers women to overcome the physical, practical, emotional and spiritual barriers of cervical cancer. It is an important component of the care of women with this disease. There are many programs and services that help meet the needs and improve the quality of life of these women and their families, especially after treatment is over.
Recovering from cervical cancer and adjusting to life after treatment differs for each woman depending on the stage of the cancer, the organs and tissues removed during the surgery, the type of treatment and many other factors. . The end of cancer treatment can lead to mixed emotions. Even if treatment is complete, there may be other issues to work out, such as coping with long-term side effects. A woman who has been treated for cervical cancer may be concerned about the following.
Self-esteem and body image
Self-esteem is how we feel about ourselves. Body image is how we perceive our own body. Cervical cancer and its treatments can affect a woman’s self-esteem and body image. This is often because cancer or treatments can cause changes in the body such as the following:
- scars
- hair loss
- changes in body weight
- sexual disturbances
- ostomy
- urinary or intestinal disorders
Some of these changes may be temporary. Others can last a long time or be permanent.
For many women, body image and how other people look is closely related to self-esteem and can be a source of real concern and distress. They may be angry or upset, afraid to go out, or fear being rejected by others, even though the effects of treatment may not be visible.
Sexuality
Many women continue to have strong, supportive relationships and satisfying sex lives after cervical cancer. If you have sexual problems with treatment for cervical cancer, there are ways to manage them.
Some side effects of treatment for cervical cancer can make sex painful or difficult:
vaginal dryness caused by radiation therapy or surgery for example
narrowing of the vagina caused by the formation of scar tissue after radiation therapy to the pelvic area or certain surgeries for vaginal cancer
menopause caused by treatment, such as radiation therapy or surgery
Women may be less interested in sex, which is common at the time of diagnosis and treatment.
When a woman starts having sex again after treatment, she may fear that it will be painful or that she may not have an orgasm. The first experiences can be disappointing. It may take a while for a couple to feel as comfortable as they used to be. Some women and their partners may need counseling to help them cope with these feelings and the effects of cancer treatments on their ability to have sex.
Fertility disorders
Fertility problems can occur after radiation therapy or chemotherapy given to treat cervical cancer. Women who have had a hysterectomy will not be able to get pregnant.
Early-stage cervical cancer may be considered to be treated to preserve the fertility of a woman who still wants to get pregnant. Before starting any treatment for cervical cancer, discuss with your healthcare team any side effects that may affect your ability to bear children after treatment and what you can do.
Lymphedema
Lymphedema is a form of swelling that occurs when lymph builds up in the tissues. It usually appears in parts of the body where a large number of lymph nodes have been removed.
You can get lymphedema in your legs if lymph nodes have been removed from your pelvis or groin. Lymphedema is more likely to occur if you have also received radiation therapy to the pelvis.
If you have lymphedema, your healthcare team may suggest ways to reduce the possible swelling and pain and prevent more lymph from building up. Lymphedema can be treated by lifting the limb so that the lymph can flow more easily, exercising, wearing compression stockings and doing physiotherapy on a regular basis. You can also ask to be referred to a healthcare professional who specializes in the treatment of lymphedema.
Ostomy care
The stoma is the opening in the surface of the body to connect an internal cavity with the abdomen. A pelvic exenteration removes the bladder, rectum, or both. A urostomy allows urine to flow out of the body, and a colostomy allows stool to pass. The person who has had their bladder and rectum removed will have these 2 ostomies.
Many people can adjust to an ostomy and live normally, although they need to learn new ways and how to care for it. Specially trained health professionals, called enterostomal therapists, teach these people how to take care of their stoma.
Worried about the cancer coming back
Many women treated for cervical cancer are concerned about the cancer coming back and it is normal. It is important to learn how to deal with these concerns in order to maintain a good quality of life.
A mental health professional, such as a social worker or therapist, can help you learn to live with and cope with a diagnosis of cervical cancer. Other members of your healthcare team can also help.
Secondary cancers
Although rare, a different, or secondary, cancer can develop after treatment for cervical cancer with radiation or chemotherapy. Although the possibility of having a secondary cancer can be scary, the benefits of treating cervical cancer with chemotherapy or radiation therapy usually far outweigh the risk of getting another cancer. Whether or not secondary cancer occurs depends on the type of chemotherapy drugs and the dose given, and whether radiation therapy is also used. Combining chemotherapy with radiation therapy (chemoradiotherapy) increases the risk of secondary cancers.
Women who receive radiation therapy to the pelvis have a low risk of developing secondary cancer in the area being treated. This region can include the colon, rectum, anus, or bladder.
Women who receive chemotherapy for cervical cancer can get secondary cancer at any time, but it usually happens within 10 years of treatment. The cancer that appears most often in women treated with chemotherapy for cervical cancer is acute myelogenous leukemia (AML).
Living a healthy lifestyle and working with your healthcare team to design a wellness plan to stay healthy can help reduce the risk of secondary cancers. Being aware of changes in your condition and reporting any problems to your doctor are also important components of follow-up after cancer treatment, as is routine screening for the early detection of secondary cancers.
Anxiety and depression
Some women with cervical cancer are very anxious or depressed during or after treatment. The level of anxiety and depression appears to be related to physical symptoms and the amount of support they feel they have from loved ones, including caregivers.
You can talk to a social worker or therapist on your healthcare team or ask to be referred to another mental health professional.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, American Cancer Society, Web MD, Cancer Center, Cleveland Clinic
Photo credit: Wikimedia Commons
Photo explanations: The appearance of cancer is signified by the crossing of the basement membrane to the underlying connective tissue by one or more cancer cells.