Male Reproductive Organs
In humans, the genital tract is closely related to the urinary tract. Male reproductive organs includes the testes, epididymis, vas deferens, seminal vesicles, prostate as well as the penis.
EXTERNAL GENITAL ORGANS in male reproductive organs
The testes are located in the bursa where they appear to hang from the spermatic cord. Ovoid in shape, the testes are about 4 cm long and 2.5 cm wide in adults. Each gland is surrounded by a membrane, the tunica vagina, derived from the abdominal peritoneum and whose extensions divide the testis into 250 to 300 lobules which each contain 3 or 4 seminiferous tubules. The seminiferous tubes then join a network of canals, the rete testis. The testes secrete male hormones or androgens, in particular testosterone which acts on the development of the genitals and secondary sexual characteristics), and they produce sperm.
Read also: Female Reproductive Organs | Female Genital System (Internal and External)
The epididymis is a duct located behind the testis (→ epididymis). It receives the sperm from it, which it directs to the vas deferens. The unrolled epididymis would measure nearly 6 meters: it takes three weeks for spermatozoa to travel through it and complete their maturation.
The vas deferens is a thin duct about 45 cm long. Its extra-abdominal part is included in the spermatic cord (pedicle containing the spermatic arteries and veins, the nerves, the ligaments that connect the testicle and the abdomen). The vas deferens enters the abdomen through the inguinal orifice to the ejaculatory duct, at the entrance to the prostate. It transports the sperm there.
The penis measures on average 10 to 12 cm at rest and 15 to 16 cm in erection. It is made up of the urethra, a conduit conveying urine during urination and semen during ejaculation, a spongy body that surrounds the urethra and two erectile organs, the cavernous bodies, which are flaccid at the state of rest, and which become rigid on erection thanks to the influx of blood. The penis ends with a swollen part, the glans, covered by a sheath of skin, the foreskin (which is removed during a circumcision).
INTERNAL GENITAL ORGANS in male reproductive organs
The seminal vesicles are two pockets located behind the prostate and the bladder, which are 5 to 7 cm long (→ seminal vesicle); they produce a viscous and alkaline seminal plasma, which will constitute the sperm with the prostatic secretions and the spermatozoa.
The ejaculatory ducts, which follow the seminal vesicles, expel semen into the urethra at the time of ejaculation.
The prostate is a gland weighing 15 to 20 grams in adults, located under the bladder neck and surrounding the urethra (→ prostate). It secretes seminal plasma, which, together with secretions from the seminal vesicles and sperm, will form sperm and activate sperm mobility.
Cowper’s glands (pea sized glands present inferior to the prostate gland), located under the prostate, produce a thick secretion that cleanses the urethra just before ejaculation.
FUNCTIONING
SPERMATOGENESIS
The production of sperm, or spermatogenesis, begins at the time of puberty and lasts throughout life, although it decreases noticeably from the age of 45 or 50. It reaches several hundred million units per day, or 50 to 100 billion per year.
It begins in the testis with the constantly renewed division of a stem cell, spermatogonia, which gives rise to new spermatogonia capable of dividing and a first daughter cell, spermatocyte I, which joins the seminiferous tube.
Sperm production
Each spermatocyte I then undergoes a first division (meiosis), which reduces the number of chromosomes from 46 to 23 (including the X and Y chromosomes), then a second division leading to four haploid daughter cells (a single chromosome of each type). They lose their previous appearance with the appearance of three structures: the head which brings together the nucleus and the acrosome rich in enzymes, an intermediate part which brings together the mitochondria, a source of energy around contractile filaments, a long tail or flagellum whose movements will be able to propel the sperm at a speed of 2 to 4 mm per minute. The complete cycle lasts 9-10 weeks, during which the sperm enters the seminal vesicles. It does not become functional until it comes into contact with seminal and prostatic secretions, at the time of ejaculation.
Each ejaculation expels between 2 and 6 ml of semen containing 60 to 300 million sperm in young adults. Environmental factors (atmospheric or food pollution, high temperature of the premises, tight clothing) would explain a regular drop in this density in the modern world. Beyond 45 years, the proportion of malformed, immobile or genetically imperfect spermatozoa increases significantly.
HORMONAL SECRETION
The interstitial cells of the testis or Leydig cells produce the main male hormone, testosterone. This production exists very early in the embryo in which it determines the evolution of the genital system towards the male type. The secretion of testosterone practically disappears during childhood and reappears at the very onset of puberty, under the stimulation of two pituitary hormones common to both sexes, LH and FSH. It peaks around the age of 20, stabilizes for a few years and then decreases very slowly.
Testosterone determines secondary sexual characteristics: development of the external genitalia, skeleton wider at the shoulders than at the pelvis, musculature, low tone of voice, growth and distribution of hair, but also aggressiveness and sexual behavior.
From the age of 40 or 50, the drop in androgen secretions participates in the physical (distribution of fat towards the abdomen, hair loss, muscle wasting) and behavioral development in men.
See the detail of neuroendocrine control of genital function and sexual differentiation of genitals during embryonic development in the General article Genital System.
Erection
The erection of the penis is a complex process conditioned by different psychological factors and the levels of male sex hormones. In response to sexual stimulation, neurotransmitter molecules are released in the corpora cavernosa that trigger vasodilation of the arteries and arterioles that supply blood to the organ, causing increased blood flow. This fact conditions the rapid filling of blood and the distension of the sinusoid system, which causes compression of the veins that drain the penis.
The final consequence is the entrapment of blood in the corpora cavernosa, making the penis increase in consistency and size, going from a flaccid state to an erection state. Very important in the process are the fibers of the parasympathetic nervous system that release nitrous oxide, which acts as a vasodilator by relaxing the smooth muscle layer of the arterial vessels.
Read also: Sagging Testicles | My balls are hanging down, what should I do?
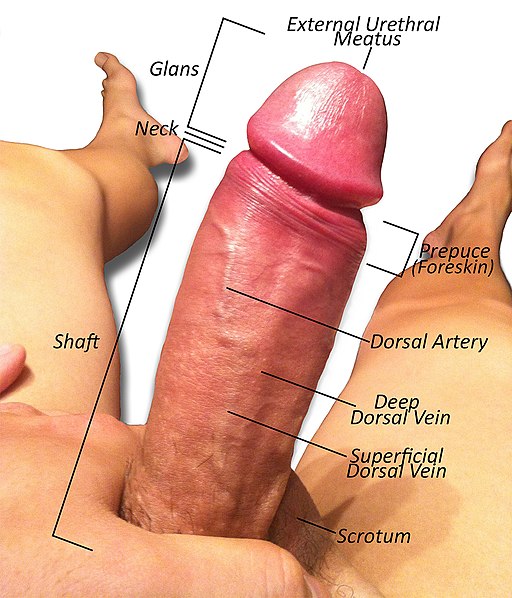
Anatomy of the penis of a fully erect uncircumcised male. Items labeled are the Scrotum, Shaft, Neck, Glans, External Urethral Meatus (Orifice), Retracted Prepuce (Foreskin), Dorsal Artery, Deep Dorsal Vein, and the Superficial Dorsal Vein. Peacebuddy420, CC BY-SA 3.0, via Wikimedia Commons
EXAMINATIONS
Many examinations explore the male reproductive system in addition to the clinical examination performed by the doctor:
– the spermogram (count of spermatozoa, study of their shape, their motility, their vitality, etc.) can make it possible to diagnose the origin of male infertility;
– testosterone blood tests explore the hormonal function of the testis;
– ultrasound focuses on describing the seminal vesicles, the prostate and the testes;
– transillumination (seen in transparency using a very strong lamp) makes it possible to detect an infectious or cancerous nucleus;
– Doppler echo studies the vascularization of the cavernous bodies, which ensure the quality of the erection.
PATHOLOGY
In addition to infertility, the main pathologies that can affect the male reproductive system are:
– testicular atrophies and ectopias (abnormal position, generally of congenital origin);
– tumors and infections of the testis and epididymis (epididymitis);
– ejaculation disorders;
– tumors, benign (adenoma) or malignant (cancer), of the prostate;
– Ureaplasma urealyticum (genital mycoplasma) | Sexually Transmitted Disease Infection
– erectile dysfunction (sexual impotence for example).
→ Testicular cancer, testicular ectopia, testicular torsion, feminizing testis, balanitis.
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Photo credit: Wikimedia Commons (CC BY-SA 3.0)



