Human heart transplant 1st surgery was performed on December 3, 1967 by Dr Barnard
Christiaan Neethling Barnard (born November 8, 1922 in Beaufort West, South Africa; † September 2, 2001 in Paphos, Cyprus) was a South African heart surgeon and pioneer in the field of heart transplants. On December 3, 1967, a South African transplant team led by Christiaan Barnard performed the world’s first heart transplant at the Groote Schuur Hospital in Cape Town . The patient Louis Washkansky survived the operation for 18 days.
In 2004, Barnard was voted second behind Nelson Mandela on the list of the 100 greatest South Africans of all time (“100 Greatest South Africans of all time”). He has been a legend not only in South Africa since the 1960s.
What is heart transplant?
A heart transplant is surgery to replace a critically ill or severely damaged heart in a person with a healthy heart from a human donor. The transplant is done if congestive heart failure or heart damage cannot be treated with drugs or other surgery. Transplantation is only for people who are at high risk of dying in the next year or two due to heart disease.
Generally, a heart transplant is considered in two types of cases. In the first place, in the event of irreversible cardiac lesions associated with coronary artery disease leading to serious heart attacks (myocardial infarction). Second, with heart muscle disease, or cardiomyopathy, which prevents the heart from contracting normally due to damage to muscle cells. More rarely, other forms of heart disease require a heart transplant, such as congenital heart disease, which is characterized by structural problems present at birth.
Read also: Heart Beat | Average resting Heart Rate by Age | Why is my heart beating too fast?
There are several risks associated with a heart transplant, including complications during and after the operation as well as death. A team of doctors and other healthcare professionals assess the condition of each patient referred to them to determine which ones might benefit from a transplant. If a patient is eligible for a heart transplant, their name is placed on a national waiting list. Patients are ranked there in order of priority, based on the severity of their condition. Thus, the sickest patients generally receive a graft first.
Description
- Before the operation, a large number of examinations are performed.
- A nurse or doctor asks the patient to sign the informed consent form, otherwise the procedure cannot take place.
- The patient undergoes general anesthesia and thus remains unconscious during the procedure.
- The patient is taken on a stretcher to the cardiac operating room.
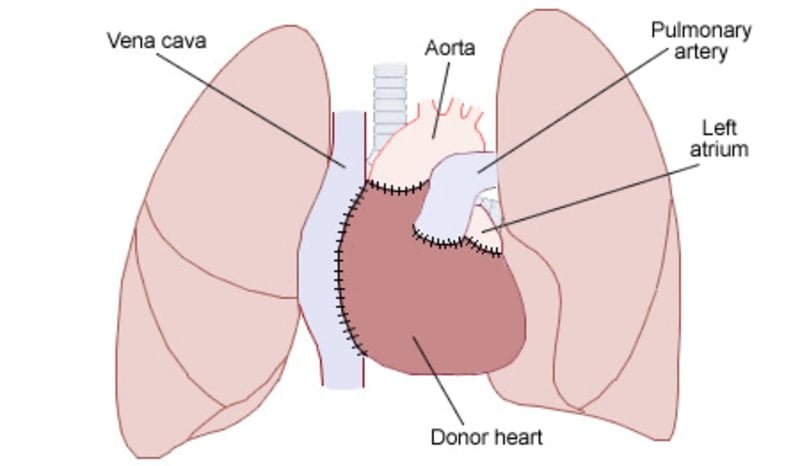
- The surgeon makes an incision in the patient’s thorax and then cuts the sternum to access the heart.
- The heart’s blood vessels are connected to a cardiopulmonary bypass machine, also called a “heart-lung machine,” which pumps blood through the patient’s body during the operation.
- Once the device is on, the heart is removed from the patient’s chest.
- Surgeons then connect the donor’s heart to the main vessels and the patient’s remaining heart tissue.
- If the new heart does not start beating automatically, a small electrical pulse is applied to start it. All the incisions are then closed.
- The patient remains in the Cardiac Surgical Intensive Care Unit (USICC) until his condition allows transfer to a regular care room. After the operation and for the rest of his or her life, the patient will need to take anti-rejection medication.
- The average length of stay in hospital following a heart transplant is 14 days.
Instructions to patients
It is important that patients waiting for a heart transplant can be reached quickly, for example by cell phone or pager. Patients who reside far from the University of Ottawa Heart Institute may be asked to provide accommodation in the Ottawa area while awaiting their transplant.
Additional Information
Heart transplant recipients need to take different medications, some of which will last for the rest of their lives. These include:
- An immunosuppressant, a drug that suppresses the body’s natural immune response, which could damage the new heart;
- Antibiotics, antivirals and fungicides to fight infections, because the immune response of transplant patients is weakened by immunosuppressants;
- Medicines to prevent coronary artery disease and to regulate blood pressure.
Following the heart transplant, blood tests and heart tissue samples (biopsies) are performed regularly to watch for signs of transplant rejection. It is important to avoid exposure to disease-causing germs as much as possible, as the patient’s immune system is not as effective as it was before the transplant.
Why are we doing it?
A heart transplant is used to treat severe and end-stage heart failure. This heart failure may be due to damage to the heart caused by:
- coronary artery disease, such as a heart attack;
- severe untreated high blood pressure (hypertensive heart disease);
- heart valve disorders;
- infections such as viruses;
- alcohol and illicit drug use;
- inherited heart disease;
- congenital heart disease (a heart defect present at birth);
- an unknown cause (idiopathic).
- In critically ill patients, a mechanical heart (mechanical assistive device) may be installed temporarily while awaiting organ donation.
How do we do it?
During this intervention:
- A machine will pump blood to the rest of your body;
- Most of the old, insufficient heart will be removed;
- The posterior walls of the two upper chambers (atria) remain in place and the new heart is attached to these remaining tissues;
- The blood vessels that enter and leave the heart are also sewn to the new heart. (As a precaution, pacemaker electrodes are also attached to the surface of the new heart and can be plugged into a pacemaker if needed.
- Before you discharge, these electrodes will be removed);
- The new heart is then given an electric shock to start beating again and the rib cage closed.
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, NHS UK, The Johns Hopkins University, American Heart Association
Photo credit: Wikimedia Commons (CC BY-SA 3.0)