Glaucoma
Glaucoma is an eye disease that causes an irremediable reduction in the field of vision.
For more information, see our fact sheet on this subject below.
It is advisable to know the symptoms of glaucoma and its risk factors as well as to undergo a regular complete ophthalmological examination, especially after the age of 40, which includes an evaluation of the optic nerve and a measurement of the intraocular pressure to detect this disease as early as possible. which can be stabilized by appropriate treatment.

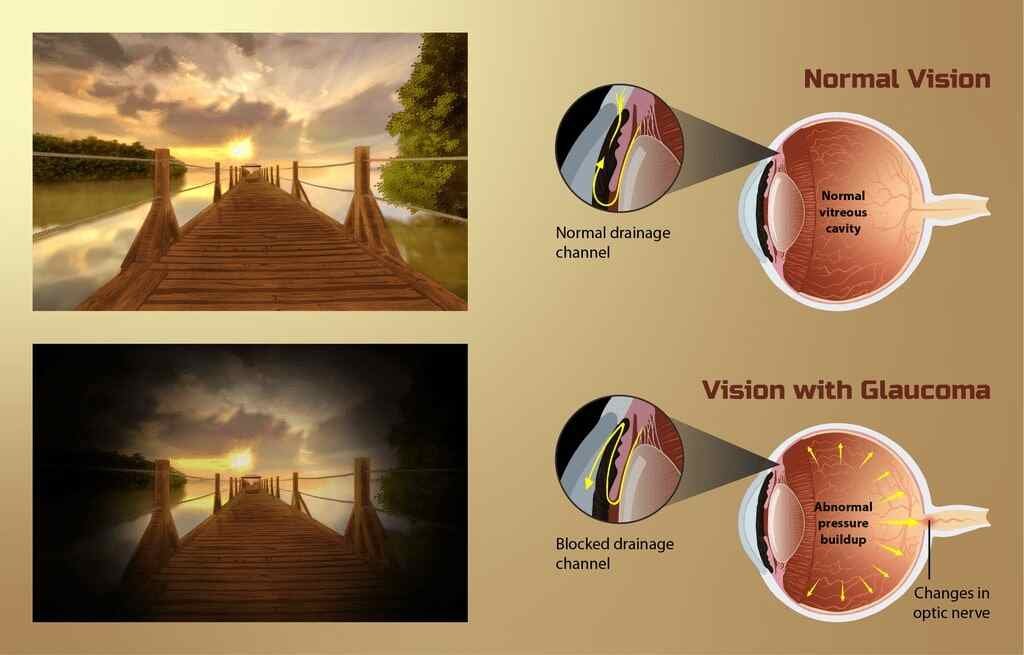
Photograph showing acute angle-closure glaucoma which is a sudden elevation in intraocular pressure that occurs when the iris blocks the eye’s drainage channel—the trabecular meshwork. Jonathan Trobe, M.D., CC BY 3.0, via Wikimedia Commons
What is glaucoma?
Glaucoma is an eye disease that interferes with the proper functioning of the optic nerve. It is the latter that transmits to the brain the visual signals that allow us to see. No one knows what causes glaucoma to develop, but increased pressure in the eye is one of the main risk factors.
Glaucoma is an eye disease that causes an irremediable reduction in the field of vision. It is the consequence of damage to the optic nerve. It is first the peripheral vision that is affected (see images below).
Most often, glaucoma is associated with increased pressure inside the eye (intraocular pressure). Normally, this should not exceed 21 millimeters of mercury (mmHg).
However, it is found that in almost 1 in 3 people, the symptoms of glaucoma appear even if the pressure in the eye is normal. A poorer blood supply to the optic nerve, caused by atherosclerosis in the vessels that irrigate this nerve, could be the cause. Whether the pressure inside the eye is too high or not, the treatment remains the same.
The different types of glaucoma
Open angle glaucoma
Accounting for 80% to 90% of cases (in Caucasians, Blacks and Hispanics), this type of glaucoma forms slowly without causing symptoms, over a period of time ranging from 10 to 20 years. The “angle” in question is that formed by the junction between the iris and the cornea. This is called the iridocorneal angle (see the interactive diagram).
Usually both eyes are affected. One of the important warning signs is the gradual rise in pressure inside the eye. Normally, this should not exceed 21 millimeters of mercury (mmHg). Intraocular pressure is detectable by eye examination.
Angle-Closure Glaucoma
Rarer (except in Asians, where it is common), it occurs following a sudden increase in pressure in the eye. This is a medical emergency. It gives rise to extreme eye pain and other noticeable symptoms, such as decreased vision and colored halos around lights.
Intraocular pressure sometimes rises to 80 mmHg. Typically, such seizures occur in the evening when the light is dim and the pupils dilate. If this type of glaucoma is not treated quickly, the person can go blind. If treated in time, the risk of blindness is greatly reduced.
Angle-closure glaucoma usually attacks one eye first, then the other within 5 years if not adequately controlled.
Two factors are required for a seizure to occur: anatomical predisposition or dilation of the pupil (the central opening of the iris, where light rays pass). It can occur following a long stay in the dark, stress or the use of drugs that dilate the pupil, such as antispasmodics, antihistamines, antidepressants and nitrates.
Acute angle closure glaucoma. Acute angle closure glaucoma of the right eye (intraocular pressure was 42 in the right eye). Note the mid sized pupil on the left that was not reactive to light and conjunctivitis. James Heilman, MD, CC BY-SA 3.0, via Wikimedia Commons
Congenital glaucoma
It can occur from birth or take a few months to show up. Most often it affects both eyes. Sometimes hereditary, it can represent an isolated problem or be explained by an ocular malformation (usually a congenital cataract) or certain rare diseases. In this case too, there is blockage of the outflow of aqueous humor.
Glaucoma: what are its causes?
Very often, we do not know why glaucoma appears. Heredity is the main risk factor. Moreover, certain anatomical characteristics could play a role.
Sometimes glaucoma is associated with a specific problem, such as: – sudden trauma to the eye; – another eye problem: cataract, pronounced myopia, chronic uveitis; – certain diseases: diabetes, hypertension, cardiovascular disorders, uncontrolled hypothyroidism.
Taking certain medications also increases the risk of glaucoma. This is the case, for example, of corticosteroids administered directly into the eyes or orally.
Remark. Corticosteroid pumps for asthma or corticosteroid creams or ointments for eczema have no effect on glaucoma.
Why is the pressure rising?
Inside the eye, between the cornea and the iris, there is a space called the anterior chamber (after having enlarged it, click on the interactive diagram below). This space is filled with a liquid called aqueous humor.
This transparent liquid performs several functions: it maintains intraocular pressure, gives its shape to the eyeball and nourishes the cornea and the lens. The aqueous humor is constantly renewed and circulates in the eye.
In most cases of glaucoma, a decrease in the excretion of aqueous humor through its outflow route occurs. Fluid excretion is either slowed down gradually, gradually leading to open-angle glaucoma, or blocked rapidly, causing angle-closure glaucoma.
Since the aqueous humor does not drain normally, the pressure inside the eye increases. The strong pressure will cause an excavation of the head of the optic nerve which alters the optical fibers of the retina and gradually destroys them. This results in a peripheral visual field disorder generally not perceived by the patient.
Glaucoma: how to diagnose it?
Here are the most commonly performed exams.
Tonometry test
This is the first test usually undertaken. The tonometer measures the pressure inside the eye. Two techniques are used: a jet of pressurized air is directed onto the open eye, this is pulsed air tonometry or after instillation of anesthetic eye drops, a flattened cone is placed on the cornea, this is pulse tonometry. flattening.
This test is both quick and painless. Normal intraocular pressure is between 8 mmHg and 21 mmHg.
Corneal thickness measurement
It is important to measure the thickness of the cornea since it influences the result obtained in the tonometry test. If the cornea is thick, the pressure is overestimated; if the cornea is thin, the pressure is underestimated.
Eye observation
Signs of optic nerve damage can be seen using a device that shines a light into the eye.
Field of view test
To assess the extent of the visual field, the person is asked to stare at a target in the center of an illuminated sphere, then a luminous point appears in different places of the visual field.
How to prevent the appearance of glaucoma?
In order to prevent the onset of glaucoma, people at higher risk (family history, diabetes, etc.) must be closely monitored.
This disease develops insidiously: many patients are unaware that they have it. A complete vision examination must be performed regularly by an ophthalmologist from the age of 40.
Basic preventive measures
- People with a higher risk of glaucoma (due to age, family history, diabetes, etc.) should have a comprehensive eye exam every year, starting in their 40s or earlier. need. The earlier the increase in intraocular pressure is detected, the more the loss of visual capacity is minimized;
- Make sure to maintain a healthy weight and normal blood pressure. Insulin resistance, which often accompanies obesity and hypertension, contributes to increased pressure inside the eyes;
- Finally, always take care to protect your eyes with goggles when practicing risky activities (handling chemicals, welding, squash, speed sports, etc.).
Measures to prevent recurrences
General precautions
- Avoid the use of certain medications, especially corticosteroids in the form of eye drops or by mouth, or consider their potential risks;
- Have a diet rich in fruits and vegetables in order to meet as many vitamin and mineral needs as possible;
- Drink small amounts of fluids at a time so as not to suddenly increase intraocular pressure;
limiting or avoiding the consumption of caffeine and tobacco is sometimes beneficial; - Exercising regularly can improve some symptoms of open-angle glaucoma, but has no effect on closed-angle glaucoma.
- In the sun, protect your eyes from ultraviolet rays by wearing glasses with tinted lenses that filter 100% of UV rays.
It is better to consult a doctor to choose the appropriate exercises. Watch out for vigorous exercise, certain yoga poses, and head-down exercises, which can increase eye pressure.
Prevent another attack of angle-closure glaucoma
Stress can trigger an acute attack of angle-closure glaucoma. We must pay attention to the factors that generate stress and try to find solutions.
Following a first angle-closure glaucoma attack, laser treatment will help prevent a recurrence. This treatment consists of making a small hole in the iris with a laser beam to allow the flow of aqueous humor trapped behind the iris. Most of the time, it is indicated to have the other eye treated as a preventive measure.
Glaucoma: treatments
Unfortunately, there is no cure. Visual acuity lost due to glaucoma cannot be recovered. The goal of treatment is therefore to prevent or slow down subsequent damage.
To do this, in many cases, it will be a question of reducing the pressure inside the eye by improving the circulation of the aqueous humor.
The ophthalmologist, the eye care doctor, will establish a treatment plan and monitor visual abilities regularly. Possible interventions include eye drops, oral medications, laser treatment and, if needed, surgery. In many cases, medication must be taken for life.
If the cause of glaucoma is identifiable, it will be important to treat it. In addition, corticosteroid therapy administered to the eyes is contraindicated in people with glaucoma.
It is therefore advisable not to undertake or to stop this type of treatment. In some cases, their use cannot be avoided. It is then necessary to obtain a very good follow-up from an ophthalmologist.
For open-angle glaucoma
Eye drops (eye drops)
They reduce the pressure in the eye. Drops are frequently prescribed because they cause fewer side effects than medications taken by mouth.
Several types of eye drops are used. Some of the most common include beta-blockers, alpha-adrenergic agents, prostaglandin analogs, carbonic anhydrase inhibitors, and miotics.
The majority of these drugs work both by reducing the production of aqueous humor in the eye and by increasing its excretion.
Adverse effects vary from one type of gout to another. These may include, for example, a dry mouth, low blood pressure, low heart rate, eye irritation, redness around the eyes or fatigue.
It is best to inform your doctor of the side effects that occur, if there are any. It is important to follow the dosage carefully. This treatment is very effective, provided it is followed daily and for life.
Oral medications
If the drops do not sufficiently reduce intraocular pressure, which is rare, oral medication may be prescribed (eg carbonic anhydrase inhibitors).
However, these drugs cause side effects more often and more pronounced than eye drops.
Laser treatment
This procedure, called trabeculoplasty, is increasingly common. Sometimes it is even offered before the use of eye drops. It can also be performed if the glaucoma worsens despite treatment or if the medication is poorly tolerated.
This laser treatment aims to help the circulation of aqueous humor in the eye. The procedure is painless and quick: it is performed in one or two 5-minute sessions. A laser beam is directed onto the trabecular meshwork (see the diagram of the internal structures of the eye above). It is unclear exactly why it lowers the pressure.
Even if a laser procedure is performed, drug treatment (most often eye drops) must still be followed for life.
Classical surgery
This eye surgery is called a trabeculectomy. The intervention aims to create a new escape route for the aqueous humor, by removing a small segment of the trabecular meshwork. Tube placement is common.
The tube directs the aqueous humor into a reservoir behind the eye. About 80% of people who have this surgery no longer need eye drops afterwards.
Other types of surgeries are being tested. Eventually, they could replace trabeculectomy. However, it will take several more years before their effectiveness can be determined. Examples include canalostomy, Ex-Press®, canaloplasty, gold implant, Glaukos iStent® and trabeculotome.
Eye Diseases and Common Eye Problems (List of eye diseases and disorders)
For angle-closure glaucoma
Emergency treatment is required. Several medications are used to quickly reduce intraocular pressure.
Once the pressure has been lowered, the ideal is to open a passageway through the iris, using a laser beam. This procedure is called peripheral iridotomy. This treatment allows the flow of the aqueous humor, in order to avoid recurrences.
Anesthetic drops are applied to the eye beforehand, as well as a contact lens (removed after the treatment). After the treatment, anti-inflammatory drops are prescribed and should be applied to the eye for a few days. Other treatments may be needed.
For congenital glaucoma
Only surgery can correct this type of glaucoma. It is practiced from the first weeks of life.
Eye Diseases and Common Eye Problems (List of eye diseases and disorders)
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, NHS UK, Mayo Clinic, American Academy of Ophthalmology, National Eye Institute
Photo credit: https://www.myupchar.com/en, source: https://www.myupchar.com/en/disease/glaucoma (CC BY-SA 4.0) via Wikimedia Commons
Photo description: depiction of vision for a Glaucoma patient. The typical pathophysiology associated with Glaucoma has been shown as well (blocked drainage channel in the eye and changes in the optic nerve).