Escherichia Coli
Escherichia Coli or “E.coli” is a bacterium found in the intestines of humans and some animals.
Escherichia coli is an intestinal bacterium responsible for food poisoning and urinary tract infections.
Escherichia coli are a family of bacteria, some of which are naturally present in the human intestine without harming it and others can cause infections. These infections, which are generally not serious, can sometimes progress to a rare but serious haemolytic uraemic syndrome in children, especially those under five years of age.
The majority of E. coli strains are harmless, only a few are pathogenic for humans. This is the case of so-called enterohaemorrhagic (EHEC) strains of E. coli. These cause bloody diarrhea and produce a powerful toxin that causes hemolytic uremic syndrome (HUS). Regularly, strains of EHEC are the cause of food poisoning through the consumption of animal products (meat or dairy products) that are poorly cooked or eaten raw. Fresh fruits and vegetables that have been in contact with EHEC may also be at risk.
How do you catch Escherichia coli?
Transmission to humans occurs mainly through the consumption of contaminated food, such as raw or undercooked minced meat, raw milk, raw vegetables and contaminated sprouted seeds.
Symptoms of Infection
Symptoms caused by EHEC (enterohaemorrhagic E. coli) appear between 3 and 8 days after infection. These are abdominal pain and diarrhea, which can progress to bloody forms (hemorrhagic colitis). Vomiting and fever may also occur.
At the same time, the toxins produced by EHEC (called Shiga-toxins because of their resemblance to those produced by Shigella dysenteriae or Shiga Bacillus) destroy the wall of blood vessels and cause clotting problems as well as high blood pressure. In 10% of infected people, the dissemination of Shiga-toxins causes a haemolytic-uremic syndrome (HUS), which is fatal in 3 to 5% of cases. The latter is characterized by impaired kidney function and a drop in the concentration of blood cells (red blood cells and platelets).
Read also: Infectious Diseases and Contagious (viruses, bacteria, parasites, fungi, protozoa)
A quarter of HUS sufferers also develop neurological complications that can lead to a state of coma. Renal sequelae that can lead to chronic renal failure several years after the HUS episode are also frequently observed.
How to diagnose E.Coli? In the urine?
The diagnosis is based on a clinical evaluation (manifestations and symptoms of the disease, aspect of the stool), a cytobacteriological examination of the urine (CBEU: CytoBacteriological Exam of Urine), if urinary tract infection (CBEU) (it is advisable to apply the rules of prior disinfection of the urethral meatus and to collect than the “medium jet” not the first), a complete blood count, a blood ionogram, the urea and creatinine levels (kidney damage) and possibly a blood culture in the presence of fever.
Coproculture (stool analysis) is useful in case of persistent diarrhoea.
Transmission
The transmission of EHEC-type pathogens mainly occurs through the consumption of contaminated food. Since the natural reservoir of EHEC is mainly the digestive tract of cattle, the food products concerned are generally raw or undercooked meat, raw milk dairy products, and more rarely raw vegetable products. Contamination can also occur during the milking or slaughter of these animals. The faeces of ruminants present in the ground, in manure and in water (ponds, streams) are also a possible source of contamination.
Human-to-human transmission of EHEC is also possible, but it occurs more rarely. In the majority of cases, it is observed in the family environment or in communities (nurseries, etc.).
Treatments
Most antibiotics are not recommended for treating EHEC infections. By destroying the bacteria, these lead to the release of Shiga-toxins in the body, which can aggravate HUS. However, treatments based on certain antibiotics, such as azithromycin, which do not lead to the release of these toxins are currently being evaluated. While waiting for their results, the therapeutic strategy of the HUS consists of compensating for the deficiencies caused by Shiga-toxins (fall in red blood cells, platelets, kidney damage) by transfusion, dialysis, and plasma exchanges.
Diarrheal episodes are treated symptomatically: patients are rehydrated, but do not take anti-diarrheals, in order to allow the elimination of the bacteria and its toxins in the stool.
► In case of intestinal infection
Dehydration linked to diarrhea and vomiting can be very important, especially in infants and the elderly. This is why, in the majority of cases, the only treatment is to drink plenty of water. If the symptoms affect a fragile person (child, elderly, chronically ill), if they include bloody diarrhea or if they last more than two days, consult a doctor. Docter can prescribe antibiotics if they think is necessary. E.coli is part of the balance of the intestinal microbiota and the prescription of antibiotics should in no case be systematic because of the risk of disturbance of the microbiota, at the origin of many pathologies.
► In case of urinary tract infection
Consult your doctor at the first symptoms, he can prescribe antibiotics and/or give you advice to make it disappear. The recommended treatment for uncomplicated E. coli cystitis in young women is oral fosfomycin in a single dose (“minute treatment”). Acquired resistance to fosfomycin remains rare, despite frequent use. This makes it possible to reduce the use of quinolones and cephalosporins which select strains resistant to these useful antibiotics in the treatment of severe infections. The treatment of pyelonephritis and bacteraemia uses 3rd generation cephalosporins, aminoglycosides or fluoroquinolones. The treatment of neonatal meningitis is based on the combination of a 3rd generation cephalosporin IV at high doses (meningeal doses) and an aminoglycoside.
Prevention and recommendations
Current knowledge does not make it possible to reduce the incidence of EHEC in cattle farms. On the other hand, through tests, it is possible to determine whether an animal is a carrier of the bacteria. If necessary, the meat can undergo a bactericidal treatment which consists of heating or irradiating it. These techniques, although effective, do not systematically guarantee the absence of EHEC in foods. To effectively protect against these infections, it is necessary to respect the application of strict hygiene practices throughout the food chain, from producer to consumer.
Personnel involved in the production and preparation of raw plant and animal products should be trained in good hygiene practices.
For consumers and cooks, most EHEC infections can be avoided by adhering to the following recommendations:
- thoroughly cook minced beef, especially for children under 5;young children should avoid consuming raw milk cheeses;
- wash fruits, vegetables and aromatic herbs, especially if they are eaten raw;
- wash your hands before preparing meals and as often as necessary;
- ensure the hygiene of equipment in the kitchen, especially when it has been in contact with raw meat, in order to avoid cross-contamination;
- separate cooked foods from raw foods;
avoid contact of very young children (under 5 years old) with farm animals, in particular cattle, sheep and their environment; - do not drink water that is not microbiologically controlled (well, spring).
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Johns Hopkins, University of Rochester Medical Center Rochester, World Health Organization (WHO)
Photo credit: HansN. / Wikimedia Commons (CC BY-SA 4.0)
Photo description:
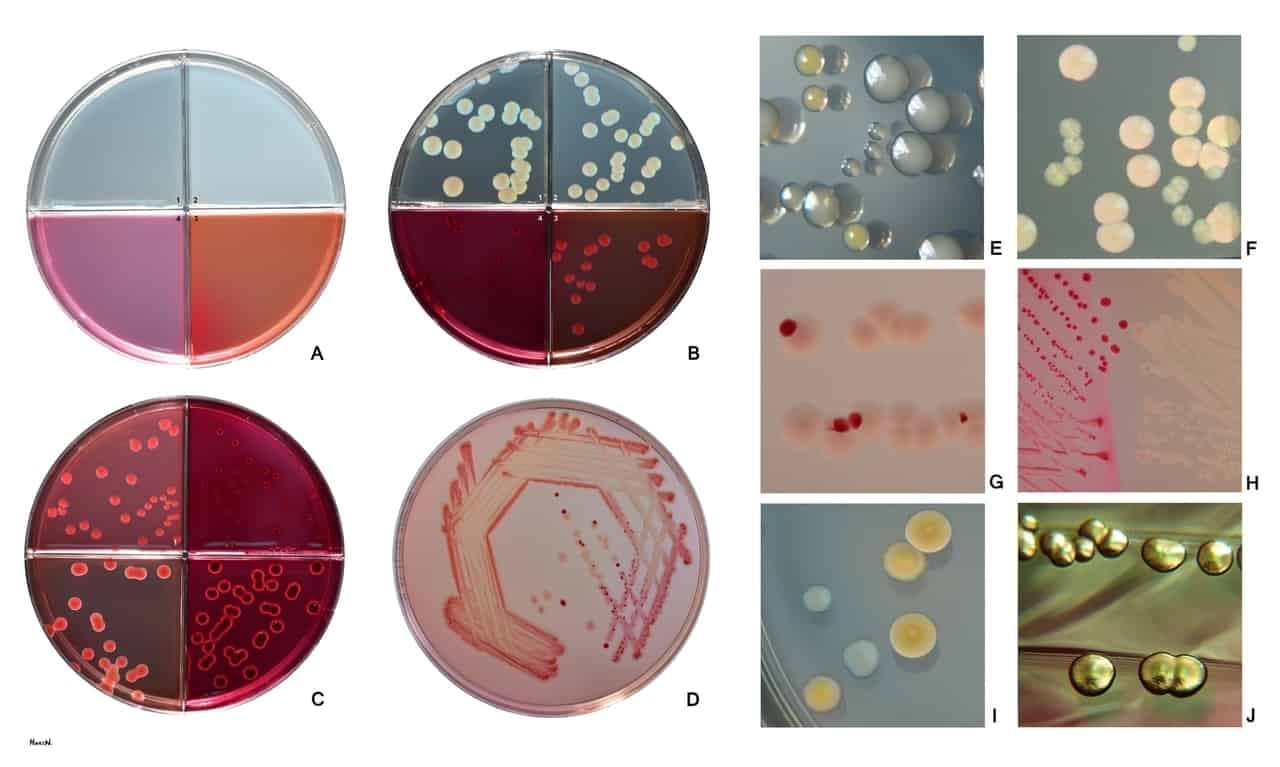
Escherichia coli grows on many commonly used cultivation media. Examples of these media are:
Fig. A1 Brain heart infusion agar (BHIA), A2 Trypticase soy agar (TSA), A3 MacConkey agar (MCA), A4 Endo agar
Fig. B shows growth of a common E. coli strain on these media. Note the different size of colonies as nutriet and selective properties of these media vary. Colonies on brain heart infusion agar (B1) are larger in comparison with colonies on trypticase soy agar (B2), MacConkey (B3) and Endo agar (B4). MacConkey (Fig. C1, C4) and Endo agar (Fig. C2, C3) represent diagnostic selective media. Both of them typically inhibit growth of Gram positive bacteria and enable differentiation between lactose positive and lactose negative bacteria (E. coli is typically lactose positive).Colonies are smallest on Endo agar as this medium has higher selectivity for Enterobacteriaceae in comparison with MacConkey agar. Size of colonies is also influenced by numbers of colonies growing on a defined surface of agar medium (higher numbers usually mean smaller colonies). (Competition for nutrients)
Fig. C E. coli growing on MacConkey (C1) and Endo agar (C2) in comparison with Klebsiella pneumoniae (C3 MacConkey, C4 Endo). Both of them are lactose positive.
Fig. D, G, H Colonies of lactose-negative and positive E. coli on MacConkey agar. E. coli strains are typically lactose positive. Colonies apperaing lactose-negative are usually delayed lactose fermentors giving positive ONPG test.
Fig. E Staphylococcus aureus (yellow), Enterococcus faecalis (small) and E. coli on trypticase soy agar after 24 h at 37°C. Seen with reflected light.
Fig. F E. coli and Pseudomonas aeruginosa (smaller greenish colonies) in mixed culture on brain heart infusion agar. 24 h, 37°C, seen with both reflected and transmitted light.
Fig. I E. coli and Klebsiella pneumoniae (larger), yellow, lactose-positive colonies on CLED agar. Bluish lactose-negative colonies of Serratia marcescens.
Fig. J Lactose-fermenting colonies of E.coli with a gold metallic sheen on Endo agar.