Celiac Disease or Gluten Intolerance
Celiac disease or gluten intolerance is a chronic and autoimmune intestinal disease linked to the ingestion of gluten, formed from the gliadin contained in certain cereal products. It occurs in genetically predisposed people.
Celiac disease is a multi-faceted autoimmune disorder that significantly impacts the lives of individuals across the globe. This comprehensive exploration delves into the intricate world of celiac disease, offering an in-depth analysis of its diverse symptoms, diagnostic methods, and a holistic approach to effective management.
Introduction: Within the realm of autoimmune disorders, celiac disease stands as a complex and often perplexing condition. Rooted in genetic predisposition, it responds to the ingestion of gluten, a ubiquitous protein found in common grains such as wheat, barley, and rye. By peeling back the layers of celiac disease, this article endeavors to provide a comprehensive understanding of its manifestations, diagnostic journey, and the empowerment of individuals living with this condition.
When eating foods containing gluten, the immune system of those affected reacts to the presence of gliadin, a gluten protein, by producing various antibodies. Celiac disease is therefore an autoimmune disease.
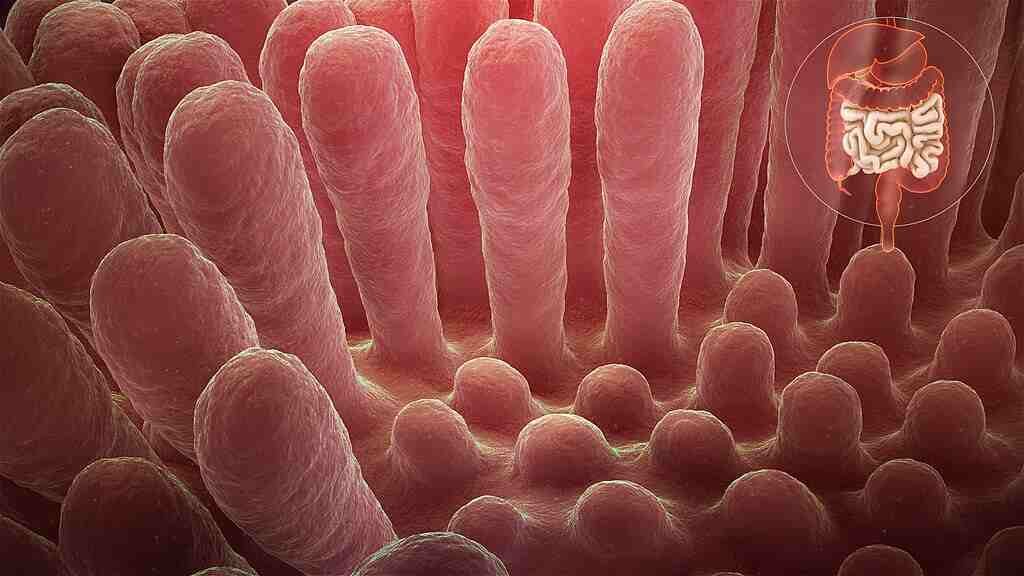
Ultimately, this abnormal autoimmune reaction causes damage to the inner wall of the intestine (atrophy of the villi of the intestinal mucosa), with two consequences:
- digestion is impaired;
- the body assimilates the majority of nutrients (proteins, fats, etc.), minerals and vitamins (iron, calcium, vitamin D, vitamin B9 or folic acid, etc.)
A common disease, gluten intolerance can give rise to minor or uncharacteristic symptoms. Unlike food allergy (and in particular gluten allergy) which cause symptoms occurring immediately after ingestion of gluten (allergen), gluten intolerance appears gradually and develops over time.
Also, gluten intolerance often goes unnoticed: in adults, it is diagnosed on average more than ten years after the first symptoms appear.
What is gluten?
Gluten is formed during the hydration of a dough and results from the association, with other elements, of two proteins present in the grain of certain cereals: gliadins (involved in celiac disease) and glutenins .
These proteins are present in:
- the different species of wheat (durum wheat, spelled, kamut);
- barley;
- the Rye ;
- hybrids of these varieties (for example, triticale, resulting from the crossing of wheat and rye).
Symptoms and Effects
Celiac disease showcases a remarkable diversity in its symptoms, defying a singular diagnostic path. Beyond its well-known gastrointestinal indicators like bloating, diarrhea, and abdominal pain, celiac disease can manifest an array of other effects. Dermatological issues, fatigue, cognitive difficulties, and even psychological disturbances can emerge. By unraveling this intricate web of symptoms, readers gain insight into the nuanced ways celiac disease impacts the body and mind.
What causes celiac disease?
The exact cause of gluten intolerance remains unknown, but it would be mainly of immune origin, with a genetic predisposition:
95% of gluten intolerant people carry one or two specific genes (HLA-DQ2 and/or HLA-DQ8).
In addition, the close family of gluten-intolerant people more often develops the disease (10% risk among first-degree relatives, ie father, mother, brothers and sisters, and any children).
However, 20% of individuals possess the genes concerned without presenting gluten intolerance.
On the other hand, certain factors favor the outbreak of this disease, such as:
- trisomy 21 (down syndrom) or other chromosomal abnormalities;
- another autoimmune disease;
- type 1 diabetes.
Diagnosis and testing
The diagnosis of celiac disease is a multifaceted process that often requires a careful amalgamation of clinical evaluation and specialized tests. While blood tests can signal the presence of celiac-related antibodies, a definitive diagnosis demands a biopsy of the small intestine. This segment delves into the significance of various diagnostic tools, guiding readers through the labyrinthine journey of obtaining a clear diagnosis.
The Role of Anti-Transglutaminase Antibodies
Diagnosing celiac disease hinges on a specific antibody found in the bloodstream: immunoglobulin A (IgA) anti-transglutaminase antibody. This test, known for its reliability, is a crucial diagnostic tool.
In adults, a positive serological test is significant. However, even in cases where celiac patients have negative antibodies, it’s advisable to consult a hepato-gastroenterologist. This specialist can perform duodenal mucosa biopsies using upper digestive endoscopy. This visual assessment confirms the diagnosis by identifying villi atrophy (partial or total) and lymphocyte proliferation, essential immune system cells.
In children, diagnosing celiac disease may sometimes bypass biopsies if symptoms are typical and blood antibody levels are notably elevated.
Celiac disease: how to treat it?
Noticed. If you think you have celiac disease, you should consult a doctor before starting a gluten-free diet. Several diseases have symptoms that can be confused with those of gluten sensitivity. And the adoption of this diet without medical advice can make the diagnosis more difficult to establish.
There is no definitive treatment for celiac disease. The only possible treatment is the gluten-free diet for life. Adopting a gluten-free diet for life most often makes it possible to completely eliminate the symptoms, treat deficiencies and prevent possible complications.
In the vast majority of cases, the tissues of the intestinal wall return to normal by following a gluten-free diet. The cutaneous symptoms (dermatitis herpetiformis) also disappear when the diet is undertaken.
This healing usually takes place in a few weeks, but can take 2 to 3 years. It is exceptional that the symptoms persist despite several months of gluten-free diet.
Living Gluten-Free
Embracing a gluten-free lifestyle is the foundation of effective management. Yet, this seemingly simple transition presents an array of hurdles. From decoding food labels to gracefully handling social gatherings and culinary adventures, adopting a gluten-free approach requires careful attention. In this segment, we provide readers with actionable tactics to seamlessly incorporate a gluten-free routine into their everyday existence. This ensures not only nutritional fulfillment but also the pleasure of culinary indulgence.
Holistic Management and Lifestyle Empowerment
Effective management of gluten-related conditions extends beyond dietary modifications. It encompasses a holistic perspective that involves gaining insight into potential nutrient gaps, considering supplementary interventions, and tending to psychological well-being, including stress and mental health. By adopting this multi-faceted approach, individuals affected by gluten-related issues can unlock their complete health potential.

Examples of sources of gluten (clockwise from top): wheat as flour, spelt, barley, and rye as rolled flakes. Photograph by Pdeitiker, Public domain, via Wikimedia Commons
What foods should I avoid on a gluten-free diet?
Cereal products with gluten
Grain products that contain gluten: wheat, bulgur (cracked durum wheat), barley, rye, spelled (a variety of wheat), kamut (a variety of wheat) and triticale (a hybrid rye and wheat). Most baked goods, pastries, pasta in all forms, cookies, breakfast cereals, crackers contain gluten.
Prepared foods
Many prepared foods: surprisingly, gluten can be found in fruit yogurts, ice cream, hot chocolate mixes, bouillon cubes, cheese sauces, low-fat cottage cheeses, sour cream, meats cans, sausages, tomato sauces, soups, peanut butter, etc.
In these foods, cereal gluten serves as a binder. It hides under several names in the ingredient lists. Things to watch out for: malt, starch (from wheat, barley, rye, etc.), hydrolyzed vegetable proteins and textured vegetable proteins. Note that seitan is a food essentially made of wheat gluten.
Beers
Beers are to be avoided, except those labeled gluten-free.
Medications
Certain medications and vitamins, the coating of which may contain gluten (starch). Choose vitamins that are hypoallergenic, wheat-free and yeast-free.
Note: alcoholic beverages obtained from malt (or derived from wheat, barley or rye) such as gin, vodka, whiskey and scotch are potentially harmful. Although distillation appears to largely remove gluten, doctors recommend avoiding these beverages as a precaution.
Beware of certain lipsticks, which may contain traces of gluten.
Some prepared foods are labeled gluten-free, with a crossed out ear of wheat logo. According to Food and Agriculture Organization (FAO) standards, these foods should not contain more than 200 parts per million (ppm) of gluten protein fractions7. It is mainly found in health food stores, but also in supermarkets.
Beware of cross contamination
In the kitchen, special care must be taken so as not to contaminate gluten-free foods. Contamination can occur when gluten-free products are prepared in unwashed dishes that have come into contact with foods containing gluten.
Also beware of exchanging utensils with people who do not follow the gluten-free diet. The toaster, for example, should be for the exclusive use of the person following a gluten-free diet.
Unfortunately, cereals that do not contain gluten sometimes become contaminated during the production, processing or packaging process. So for more security, it is advisable to favor products labeled gluten-free.
The special case of oats
Regular oat cereal does not contain gluten. On the other hand, there is a high risk of cross-contamination since oats are very often grown, transported or ground in the same environments as cereals or food products containing gluten.
The Quebec Celiac Foundation (FQMC) suggests that uncontaminated/gluten-free oats be introduced only after the normalization of anti-transglutaminase antibodies. This normalization takes between 6 months to 2 years after the start of a strict gluten-free diet.
Gluten-free products: not all good for your health
It is important, when starting a gluten-free diet, to adequately replace the foods that we have excluded from our diet. The impact of these restrictions on protein, vitamin, mineral and other nutrient intakes can be negative. It is necessary to see how to replace the essential nutrients contained in foods with gluten traditionally consumed.
For example, breads and cereals are often fortified with iron and vitamin B (especially B9/folic acid) while gluten-free breads and cereals are not. Gluten-free products are often low in fiber and protein and high in sugars and additives. Be careful to choose your replacement products carefully.
Gluten-free diet: what foods to eat
Dietary changes and a gluten-free diet may significantly alleviate, and sometimes completely eliminate, the troublesome symptoms of the condition.
Gluten-Free Food Options (gluten free version)
Nowadays, gluten-free versions of foods like bread, biscuits, pastries, and pasta are not only available in specialty stores but also on supermarket shelves. However, it’s important to be cautious. Some gluten-free industrial products may use additives or chemicals to compensate for flavor and texture. Reading labels carefully and cooking raw ingredients at home is recommended over relying on ready-to-eat meals.
Naturally Gluten-Free Choices
The good news is that many foods are naturally free of gluten if not processed industrially:
- All fruits and vegetables without exception.
- Animal proteins like meat, fish, seafood, and eggs.
- Dairy products such as yogurt, cottage cheese, and cheese.
- Gluten-Free Carbohydrate Sources
While less common in our diet, there are several plant-based sources of naturally gluten-free carbohydrates:
- Cereals: corn, rice, millet, flax, oats.
- Pseudo-cereals: quinoa, buckwheat, sesame.
- Tubers and roots: potato, sweet potato, yam, cassava, parsnip.
- Legumes: chickpeas, lentils, dried beans, broad beans.
- Certain fruits: banana, chestnut, pumpkin.
Conclusion
Long-Term Implications and Future Outlook
Unmanaged celiac disease can trigger a cascade of long-term complications, from impaired nutrient absorption and osteoporosis to heightened vulnerability to other autoimmune disorders. By emphasizing the importance of consistent medical oversight, adherence to a gluten-free diet, and a proactive stance on health maintenance, this section underlines the steps individuals can take to mitigate risks and optimize their future well-being.
Navigating the Landscape of Celiac Disease
Celiac disease is a dynamic and intricate condition that necessitates unwavering attention, knowledge, and proactive management. By embarking on this comprehensive exploration, individuals impacted by celiac disease, alongside their families and healthcare providers, can embark on a journey of informed decision-making, resilient adaptation, and empowered living.
Incorporating scientific insights, real-life anecdotes, and practical guidance, this article serves as an indispensable resource for the celiac community, ensuring that the complexities of this condition are demystified and navigated with confidence and competence.
Sources: Health Line, Johns Hopkins, PinterPandai, National Center for Biotechnology Information (NCBI)
Photo credit: www.scientificanimations.com, CC BY-SA 4.0, via Wikimedia Commons
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.