Shedding in Neurology: What the Brain “Releases” and Why It Matters
One-sentence takeaway (remember this!)
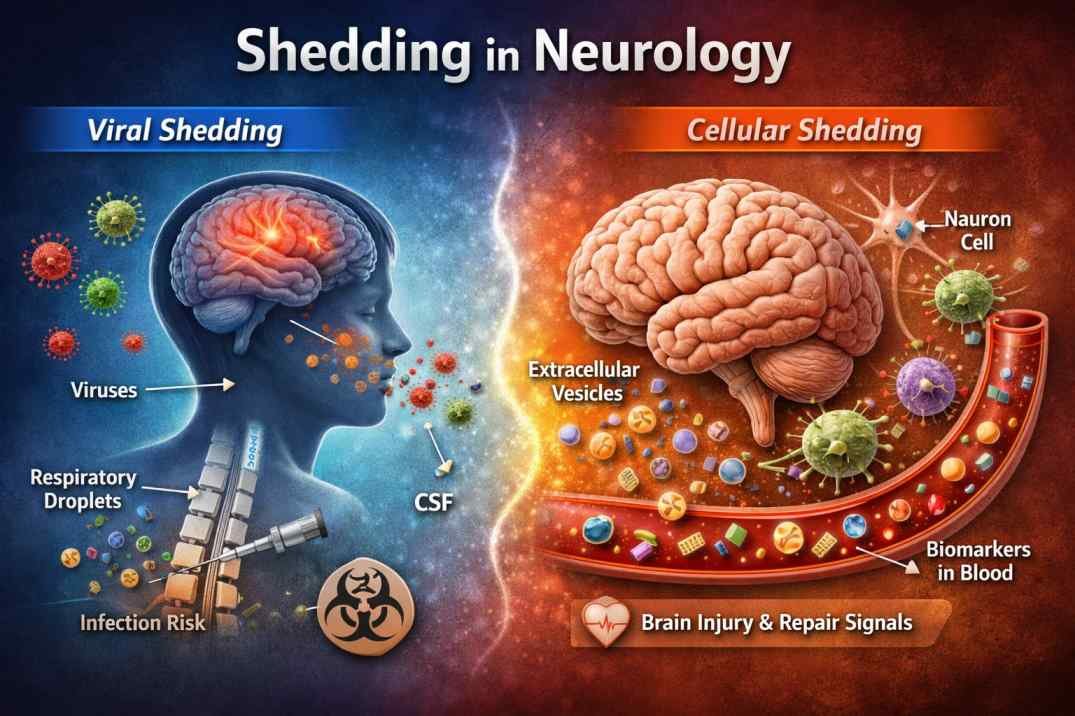
In neurology, “shedding” means the brain or nervous system releasing something measurable—either viruses or microscopic cell particles—that tells us what is happening inside the body.
What does “shedding” mean in neurology?
In medical science, shedding means the release of biological material from cells into body fluids such as blood, cerebrospinal fluid (CSF), or respiratory secretions.
In neurology, shedding appears in two real and scientifically accepted contexts:
- Viral shedding → related to infections that can affect the nervous system
- Cellular (microparticle / extracellular vesicle) shedding → related to brain injury, stroke, inflammation, and neurodegeneration
Same word. Very different meanings.
Context is everything.
1. Viral shedding and the nervous system
What is viral shedding?
Viral shedding is the process by which a virus exits an infected person and becomes detectable (and sometimes contagious).
This usually happens through:
- Nasal or throat secretions
- Saliva
- In some cases, cerebrospinal fluid (CSF)
Why neurologists care
Some viruses are neurotropic, meaning they can affect the brain or nerves:
- Encephalitis
- Meningitis
- Post-viral neurological syndromes
Understanding when and how long a virus is shed helps doctors:
- Estimate contagion risk
- Time isolation or treatment
- Protect vulnerable neurological patients
Easy example
A patient has a viral infection that can affect the brain.
Shedding tells doctors when the virus is still active and risky.
2. Cellular shedding: the brain leaving “fingerprints” in the blood
What is cellular shedding?
Brain cells, blood vessels, and immune cells can release microscopic membrane-bound particles called:
- Extracellular vesicles
- Microparticles
- Exosomes
These particles carry:
- Proteins
- RNA
- Lipids
They act like biological messages.
Shedding after stroke: a powerful example
After an ischemic stroke, studies show increased shedding of microparticles from:
- Endothelial (blood vessel) cells
- Immune cells
- Neural precursor cells
These particles can remain detectable for weeks.
Why this matters
Doctors can potentially:
- Detect brain injury from a blood test
- Monitor inflammation and repair
- Predict recovery or complications
This idea is often called a “liquid biopsy” of the brain.
Memory hook
“After stroke, the brain leaves clues in the blood.”
Shedding in neurodegenerative diseases
Research is actively exploring whether neuron-derived vesicles in blood may help study:
- Alzheimer’s disease
- Parkinson’s disease
- Other neurodegenerative conditions
Important:
This is real science, but not yet routine clinical practice. Validation is ongoing.
The 3-line model you’ll remember
Shedding in neurology = release with meaning
- Viral shedding → when infection can spread
- Cellular shedding → signals of injury, inflammation, or repair
- Context defines the interpretation
Common misunderstandings (quick clarity)
- ❌ Shedding ≠ always contagious
- ❌ Shedding ≠ hair loss
- ✅ Shedding = measurable biological release
Why this topic is going viral (and why it should)
- Non-invasive diagnostics
- Precision neurology
- Early disease detection
- Personalized medicine
Shedding turns invisible brain processes into measurable signals.
Trusted scientific sources
- Mayo Clinic – Viral shedding explained
https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-qa-podcast-what-is-viral-shedding/ - CDC (Emerging Infectious Diseases) – Infectious virus shedding study
https://wwwnc.cdc.gov/eid/article/28/5/22-0197_article - NCBI (PubMed Central) – Extracellular vesicles and brain disease (review)
https://pmc.ncbi.nlm.nih.gov/articles/PMC4729528/ - Frontiers in Immunology – Microparticles / extracellular vesicles after stroke (review)
https://www.frontiersin.org/articles/10.3389/fimmu.2019.02747/full - Alzheimer’s & Dementia (Wiley) – Neuron-derived extracellular vesicles in Alzheimer’s research
https://alz-journals.onlinelibrary.wiley.com/doi/full/10.1002/alz.14497
Other sources: PinterPandai, American Academy of Neurology